Diabetes insipidus (DI) is a rare disorder characterized by the inability of the body to properly regulate fluid balance, leading to excessive thirst and urination. While it shares a part of its name with the more common diabetes mellitus, the two conditions are distinct. Diabetes insipidus is caused by a deficiency of, or insensitivity to, antidiuretic hormone (ADH), also known as vasopressin. Managing diabetes insipidus involves addressing the underlying cause and providing symptomatic relief through medication. In this blog, we will delve into the various medications used in the treatment of diabetes insipidus, their mechanisms of action, and potential side effects.
Contents
Understanding the Role of Antidiuretic Hormone (ADH)
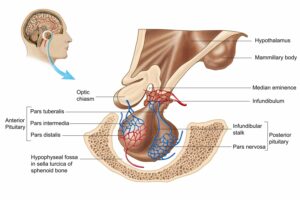
Antidiuretic Hormone (ADH), also known as vasopressin, is a crucial hormone that plays a central role in regulating water balance within the body. Produced by the hypothalamus, a region in the brain, ADH is stored and released by the pituitary gland. Its primary function is to control the amount of water reabsorbed by the kidneys, influencing urine concentration and, consequently, fluid balance.
Understanding the role of ADH is essential to comprehend conditions like diabetes insipidus, where disruptions in its function can lead to significant health issues.
Water Balance Regulation:
- ADH acts on the kidneys, specifically on the renal tubules, to increase water reabsorption. This occurs in response to changes in blood osmolality, which is the concentration of solutes in the blood.
- When blood osmolality increases, indicating dehydration or a higher concentration of solutes in the blood, the hypothalamus stimulates the release of ADH.
- ADH then acts on the kidneys, promoting the reabsorption of water back into the bloodstream, reducing urine volume, and concentrating the urine.
Osmoreceptors and Thirst Regulation:
- Osmoreceptors, specialized cells in the hypothalamus, sense changes in blood osmolality. When osmolality rises, osmoreceptors signal the hypothalamus to release ADH.
- ADH not only influences water reabsorption but also triggers the sensation of thirst. Thirst prompts an individual to drink fluids, further contributing to fluid balance regulation.
List of Medications for Diabetes Insipidus
Let’s delve into an assertive and proactive exploration of medications for diabetes insipidus, showcasing a bold approach to understanding and managing this condition.
1. Desmopressin (DDAVP)
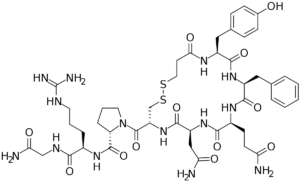
Desmopressin, commonly known by its trade name DDAVP, is a synthetic analog of antidiuretic hormone (ADH) or vasopressin. It is a key medication in the management of diabetes insipidus (DI), a condition characterized by impaired water balance due to deficient or ineffective ADH.
Mechanism of Action: Desmopressin primarily acts on the kidneys to enhance water reabsorption, reducing urine volume and increasing urine concentration. Unlike natural vasopressin, desmopressin is more selective for the V2 receptors in the renal collecting ducts, minimizing its vasoconstrictive effects on blood vessels.
In individuals with central diabetes insipidus, where ADH production or release is deficient, desmopressin serves as a synthetic replacement. By mimicking the action of ADH, it promotes water retention and reduces excessive urine output.
Administration: Desmopressin is available in various formulations, including oral tablets, intranasal sprays, and injectable forms. The choice of administration depends on the severity of the condition, patient preferences, and the response to treatment.
- Oral Tablets: Desmopressin tablets are convenient for daily use. The dosage is carefully titrated based on individual needs to achieve optimal control of symptoms. It is essential to take the medication as prescribed, with or without food, and maintain adequate fluid intake.
- Intranasal Spray: The intranasal formulation involves spraying the medication into the nostrils. This allows for rapid absorption through the nasal mucosa. Intranasal desmopressin is particularly useful when an immediate onset of action is necessary.
- Injectable Form: In severe cases or situations where other formulations are not practical, desmopressin can be administered through injection, either intramuscularly or subcutaneously. Injectable forms are usually reserved for hospital settings or under the guidance of healthcare professionals.
2. Thiazide Diuretics (e.g., Hydrochlorothiazide)
Introduction: Thiazide diuretics, such as hydrochlorothiazide, are commonly employed in the treatment of diabetes insipidus, particularly in cases of nephrogenic diabetes insipidus where the kidneys do not respond adequately to antidiuretic hormone (ADH).
Mechanism of Action: Hydrochlorothiazide works by inhibiting sodium and chloride reabsorption in the distal convoluted tubules of the kidneys. By doing so, it indirectly enhances water reabsorption. The diuretic effect of hydrochlorothiazide helps decrease urine volume, relieving the excessive urination characteristic of diabetes insipidus.
Administration: Hydrochlorothiazide is typically administered orally in the form of tablets. The dosage is carefully determined based on individual patient needs and response to treatment. It is often used in combination with other medications to achieve optimal results.
3. Indomethacin
Introduction: Indomethacin, a nonsteroidal anti-inflammatory drug (NSAID), is sometimes used in the treatment of nephrogenic diabetes insipidus. Its mechanism of action involves influencing the responsiveness of the kidneys to antidiuretic hormone (ADH).
Mechanism of Action: Indomethacin inhibits the production of prostaglandins, which play a role in regulating the kidneys’ response to ADH. By reducing prostaglandin synthesis, indomethacin can enhance the kidneys’ ability to concentrate urine.
Administration: Indomethacin is typically administered orally in the form of capsules or as a suppository. The dosage is determined based on the severity of the condition and individual patient response.
Certainly! Given the character limitations, I’ll provide detailed descriptions of two more medications commonly used in the treatment of diabetes insipidus:
4. Amiloride
Introduction: Amiloride is a potassium-sparing diuretic that is occasionally used in the management of nephrogenic diabetes insipidus. It works by affecting the reabsorption of sodium and water in the kidneys, contributing to a reduction in urine volume without causing significant potassium loss.
Mechanism of Action: Amiloride acts on the distal tubules of the kidneys, specifically inhibiting the epithelial sodium channels (ENaC). By blocking these channels, the reabsorption of sodium is reduced, leading to increased water excretion. Importantly, unlike other diuretics, amiloride helps to spare potassium, minimizing the risk of hypokalemia.
Administration: Amiloride is typically administered orally in the form of tablets. The dosage is individualized based on the patient’s response to the medication, with close monitoring of renal function and electrolyte levels.
5. Vasopressin Receptor Agonists (Vaptans) – Tolvaptan

Introduction: Vaptans, such as tolvaptan, are a relatively newer class of medications used in the treatment of hyponatremia associated with conditions like syndrome of inappropriate antidiuretic hormone secretion (SIADH). While not a primary treatment for diabetes insipidus, vaptans may be considered in certain cases.
Mechanism of Action: Tolvaptan selectively antagonizes the effects of vasopressin by binding to the V2 receptors in the renal collecting ducts. This leads to increased water excretion, allowing for the correction of hyponatremia.
Administration: Tolvaptan is administered orally in the form of tablets. The dosage is carefully titrated based on the patient’s response and is generally initiated under close medical supervision.
6. Chlorpropamide
Introduction: Chlorpropamide is an oral sulfonylurea medication that has been historically used in the treatment of diabetes insipidus. It is primarily employed in cases of central diabetes insipidus where antidiuretic hormone is deficient (ADH) production.
Mechanism of Action: The exact mechanism by which chlorpropamide exerts its effects in diabetes insipidus is not entirely understood. However, it is believed to enhance the release of ADH from the posterior pituitary gland, effectively increasing water reabsorption in the kidneys.
Administration: Chlorpropamide is administered orally in the form of tablets. The dosage is carefully adjusted based on the patient’s response and is typically taken once daily.
7. Lithium
Introduction: Lithium, a mood-stabilizing medication commonly used in the treatment of bipolar disorder, has been associated with the development of nephrogenic diabetes insipidus. This type of diabetes insipidus is characterized by the kidneys’ reduced responsiveness to ADH.
Mechanism of Action: Lithium interferes with the ability of the renal tubules to respond to ADH, reducing the kidneys’ capacity to concentrate urine. The exact mechanism is complex and not fully elucidated, but it involves changes in the responsiveness of the collecting ducts to ADH.
Administration: Lithium is typically administered orally in the form of tablets or capsules. The dosage is individualized based on the patient’s response to the medication, and regular monitoring of lithium levels in the blood is essential.
8. Diuretics
Introduction: Diuretics, commonly known as water pills, are a diverse class of medications that increase urine production and reduce fluid retention. While diuretics are not the first-line treatment for diabetes insipidus, they may be used in certain cases to manage symptoms.
Mechanism of Action: Diuretics work by increasing the excretion of sodium and water by the kidneys. By enhancing urine production, diuretics indirectly reduce blood volume and subsequently decrease urine concentration.
Types of Diuretics:
- Thiazide Diuretics: Thiazides, such as hydrochlorothiazide, are sometimes used in nephrogenic diabetes insipidus. They promote water reabsorption by inhibiting sodium reabsorption in the distal tubules of the kidneys.
- Loop Diuretics: These diuretics, like furosemide, act on the loop of Henle in the kidneys, inhibiting sodium reabsorption. They are less commonly used in diabetes insipidus due to their powerful diuretic effect.
Administration: Diuretics are typically administered orally, and the choice of the specific type and dosage depends on the severity and type of diabetes insipidus. Thiazides are more commonly prescribed for their milder diuretic effects.
9. Clofibrate
Introduction: Clofibrate, a fibric acid derivative, has been historically used in the treatment of diabetes insipidus. It is particularly considered in cases where other treatments have not been effective.
Mechanism of Action: The exact mechanism by which clofibrate affects diabetes insipidus is not fully understood. It is believed to have an antidiuretic effect by influencing water reabsorption in the kidneys.
Administration: Clofibrate is typically administered orally in the form of tablets. The dosage is adjusted based on the patient’s response, with regular monitoring of symptoms and potential side effects.
10. Methoxyflurane
Introduction: Methoxyflurane is an inhalational anesthetic that has been used in the management of central diabetes insipidus. While not a primary treatment, it has been employed in specific situations to reduce excessive thirst and urine output.
Mechanism of Action: The exact mechanism by which methoxyflurane affects diabetes insipidus is not entirely clear. However, it is believed to have an antidiuretic effect, potentially influencing the release or response to antidiuretic hormone (ADH) in the kidneys.
Administration: Methoxyflurane is administered through inhalation. The patient inhales the vaporized form of the medication using a specialized inhaler device. The dosage is carefully adjusted based on the patient’s response and the severity of symptoms.
Considerations To Take Before Medications for Diabetes Insipidus

Before initiating medications for diabetes insipidus, healthcare providers carefully evaluate several considerations to ensure safe and effective treatment. Here are key considerations:
1. Accurate Diagnosis:
Before starting any medication, a precise diagnosis is crucial. Diabetes insipidus can have different causes, such as central diabetes insipidus due to insufficient ADH production or nephrogenic diabetes insipidus caused by kidney resistance to ADH. Understanding the specific type and underlying cause guides the choice of medication.
2. Underlying Conditions:
Assessing and addressing any underlying conditions is paramount. Diabetes insipidus can be secondary to other health issues, such as tumors, trauma, or certain medications. Identifying and managing these underlying factors is essential for comprehensive care.
3. Patient’s Overall Health Status:
Taking into account the patient’s overall health, including any existing medical conditions and medications, is essential. Some medications may have interactions or contraindications that need careful consideration to prevent adverse effects.
4. Pregnancy and Lactation:
For female patients, the potential impact of medications on pregnancy and lactation must be considered. Certain medications may pose risks during pregnancy or while breastfeeding, and alternative treatment options may need to be explored.

