Hypoglycemia, commonly known as low blood sugar, is a condition that occurs when the level of glucose in the blood drops below normal. This can be a concerning and potentially dangerous situation, especially for individuals with diabetes. This blog will explore the causes, symptoms, and most importantly, the various treatment strategies available for managing hypoglycemia.
Contents
Symptoms and Causes of Hypoglycemia
Hypoglycemia occurs when blood sugar levels drop below normal levels, typically below 70 milligrams per deciliter (mg/dL). This condition can be caused by various factors and can lead to a range of symptoms. Here are some common symptoms and causes of hypoglycemia:
Symptoms:
- Shakiness or tremors: Feeling shaky or trembling, especially in the hands, is a common symptom of low blood sugar.
- Sweating: Hypoglycemia can cause excessive sweating, even when the environment is not hot.
- Hunger: A sudden onset of hunger, even after eating a meal not too long ago, can be a sign of low blood sugar.
- Irritability or mood changes: Hypoglycemia can affect mood, leading to irritability, anxiety, or even confusion.
Causes:
- Diabetes medications: Hypoglycemia is most commonly associated with diabetes treatment, particularly if a person with diabetes takes too much insulin or other glucose-lowering medications.
- Skipping meals or inadequate food intake: Not eating enough food or skipping meals can lead to hypoglycemia, especially in individuals with diabetes or those prone to low blood sugar levels.
- Increased physical activity: Intense or prolonged physical activity can deplete glucose stores in the body, leading to hypoglycemia, especially if adequate carbohydrates are not consumed to replenish them.
Different Hypoglycemia Treatment Methods
While there are numerous ways to address hypoglycemia, each method plays a crucial role in managing low blood sugar levels effectively. Let’s delve into detailed explanations of ten different hypoglycemia treatment methods:
Immediate Carbohydrate Intake
Immediate carbohydrate intake stands as a frontline and critical strategy in the treatment of hypoglycemia, particularly for individuals with diabetes. This approach is rooted in the need to swiftly elevate blood sugar levels to alleviate symptoms and prevent the progression of hypoglycemia.
Mechanism of Action:
The rationale behind immediate carbohydrate intake lies in the rapid conversion of ingested carbohydrates into glucose. Glucose is the primary fuel for the body, especially the brain, and quickly replenishing its levels helps counteract the effects of low blood sugar.
Sources of Rapid-Acting Carbohydrates:
- Glucose Tablets: Specifically designed for this purpose, glucose tablets provide a concentrated source of glucose that is rapidly absorbed into the bloodstream. They are portable, easy to carry, and offer a precise amount of glucose to address the immediate need.
- Fruit Juices: Natural fruit juices, such as orange or apple juice, contain simple sugars that can be quickly absorbed. The fructose and glucose content in these juices provides a fast-acting source of carbohydrates.
- Regular Soda: Non-diet soda, with its high sugar content, can be an effective choice for rapidly raising blood sugar levels. The carbonation can also aid in faster absorption.
- Candy or High-Sugar Snacks: Candy, particularly those containing glucose or sucrose, serves as a convenient option. High-sugar snacks, such as raisins or a small piece of chocolate, can also provide a quick energy boost.
Glucagon Injection
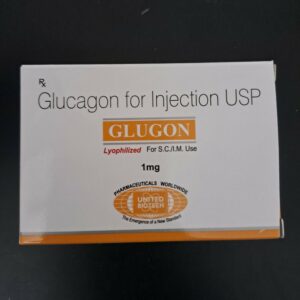
intervention in the treatment of severe hypoglycemia, especially when the affected individual is unconscious or unable to consume oral carbohydrates. Glucagon, a hormone produced by the pancreas, stimulates the liver to release stored glucose into the bloodstream, rapidly raising blood sugar levels.
Mechanism of Action:
- Liver Stimulation: Glucagon acts on the liver, prompting the conversion of stored glycogen into glucose. This newly released glucose is then released into the bloodstream, providing a quick and substantial increase in blood sugar levels.
Indications for Use:
- Severe Hypoglycemia: Glucagon is typically used when an individual with diabetes experiences severe hypoglycemia, characterized by unconsciousness or an inability to swallow.
- Unconsciousness or Inability to Swallow: In situations where the affected person is unconscious or unable to consume oral carbohydrates, a glucagon injection becomes a crucial alternative to raise blood sugar levels promptly.
Adjusting Medications
Adjusting medications is a fundamental and personalized approach to managing hypoglycemia, particularly in individuals with diabetes. This method involves modifying the dosage, timing, or type of insulin or other hypoglycemic medications to maintain blood sugar levels within a target range and prevent episodes of low blood sugar.
Types of Medication Adjustments:
Insulin Dosage Adjustments:
- Basal Insulin: Modifying the dosage of long-acting or basal insulin can impact fasting blood sugar levels. This adjustment addresses the body’s need for a steady supply of insulin between meals and overnight.
- Bolus Insulin: Adjusting rapid-acting or bolus insulin doses, especially about meals, helps manage postprandial glucose levels. This can involve changes in the insulin-to-carbohydrate ratio or correction factors.
Oral Hypoglycemic Agents:
- Adjustments to oral medications may include changes in dosage or the addition of new medications. Some medications stimulate insulin production, while others improve insulin sensitivity or reduce glucose absorption in the digestive tract.
Combination Therapies:
- For individuals on multiple medications, optimizing the combination and dosage of different classes of medications may be necessary. This approach aims to achieve optimal glycemic control while minimizing the risk of hypoglycemia.
Continuous Glucose Monitoring (CGM)
Continuous Glucose Monitoring (CGM) has emerged as a revolutionary tool in the management of diabetes, playing a pivotal role in not only monitoring blood glucose levels but also preventing and treating hypoglycemia. This advanced technology provides real-time data, enabling individuals and healthcare professionals to make informed decisions to maintain optimal blood sugar levels.
Mechanism and Technology:
- Sensor Placement: CGM involves the insertion of a tiny sensor under the skin, usually on the abdomen, which continuously measures glucose levels in the interstitial fluid.
- Real-Time Data: The sensor communicates with a receiver or a smartphone app, providing real-time updates on blood glucose levels. Some systems can even predict glucose trends, giving users valuable insights into their metabolic patterns.
Preventing Hypoglycemia:
- Alerts and Alarms: CGM systems have customizable alerts and alarms that notify individuals when their blood glucose levels approach or drop below predefined thresholds. This early warning system allows for proactive intervention to prevent hypoglycemia.
- Trend Analysis: By analyzing glucose trends over time, CGM users can anticipate potential hypoglycemic episodes. Identifying patterns, such as recurrent lows during specific times of the day, enables adjustments to treatment plans to mitigate the risk.
Balanced and Regular Meals

Balanced and regular meals are essential components of managing blood sugar levels, especially for individuals with diabetes. Adopting a structured and nutritious approach to meals contributes to stable glucose levels throughout the day. Here are key points highlighting the importance of balanced and regular meals in diabetes management:
Consistent Meal Timing:
- Eat meals at regular intervals throughout the day to help stabilize blood sugar levels.
- Aim for three main meals and incorporate healthy snacks between meals to prevent prolonged periods without food.
Carbohydrate Distribution:
- Spread carbohydrate intake evenly across meals to avoid large spikes in blood sugar after eating.
- Choose complex carbohydrates with a lower glycemic index, such as whole grains, legumes, and vegetables, for sustained energy release.
Protein Inclusion:
- Include a source of lean protein (e.g., poultry, fish, tofu, legumes) in each meal to promote satiety and help regulate blood sugar levels.
- Protein-rich foods have a minimal impact on blood glucose compared to carbohydrates.
Healthy Fats:
- Incorporate sources of healthy fats, such as avocados, nuts, and olive oil, to enhance the overall nutritional profile of meals.
- Healthy fats contribute to a feeling of fullness and can help mitigate rapid spikes in blood sugar.
Portion Control:
- Pay attention to portion sizes to avoid overeating, which can lead to post-meal hyperglycemia.
- Use smaller plates and bowls to help with portion control and prevent excessive calorie intake.
Avoiding Excessive Alcohol Consumption
Avoiding excessive alcohol consumption is a crucial aspect of hypoglycemia management, particularly for individuals with diabetes. Alcohol can significantly impact blood sugar levels and interfere with the body’s ability to regulate glucose. Here are key points highlighting the importance of limiting alcohol intake in the context of hypoglycemia treatment:
Hypoglycemia Risk:
- Alcohol consumption can lead to hypoglycemia, especially if consumed on an empty stomach or in large quantities.
- The liver’s primary function is to regulate blood sugar levels by releasing glucose when needed. However, when the liver is metabolizing alcohol, it may be less effective in this role, contributing to low blood sugar.
Delayed Symptoms Recognition:
- Alcohol consumption can mask the early symptoms of hypoglycemia, such as shakiness or irritability. Individuals may not recognize the signs of low blood sugar, leading to delayed or inadequate treatment.
Interference with Glucose Production:
- Alcohol can impair the liver’s ability to produce glucose, further exacerbating the risk of hypoglycemia.
- For individuals with diabetes who are already at risk of glucose fluctuations, the additional impact of alcohol on liver function can pose significant challenges.
Snacking Before Physical Activity
Snacking before physical activity is a strategic and proactive approach to prevent hypoglycemia, especially for individuals with diabetes. Engaging in exercise can lower blood sugar levels, and consuming a balanced snack beforehand helps ensure a stable source of energy during the activity. Here are key points highlighting the importance of snacking before physical activity as a hypoglycemia treatment:
Preventing Exercise-Induced Hypoglycemia:
- Role of Physical Activity in Blood Sugar Regulation: Exercise enhances insulin sensitivity and can lead to a rapid uptake of glucose by muscles, potentially causing a drop in blood sugar levels.
- Timing of Snack Consumption: Consuming a snack approximately 30 minutes to an hour before physical activity provides the body with a readily available source of glucose.
Balanced Snack Components: The pre-exercise snack should be balanced, containing a combination of carbohydrates, protein, and a small amount of healthy fats. Carbohydrates provide quick energy, while protein and fats contribute to sustained energy release.
Choosing Suitable Snacks:
- Carbohydrate Options: Choose complex carbohydrates with a moderate to high glycemic index to provide a steady release of glucose. Examples include whole grains, fruits, or energy bars.
- Protein Sources: Include a source of protein to support muscle function during physical activity. This can be in yogurt, nuts, seeds, or a protein bar.
- Healthy Fats: A small amount of healthy fats, such as those found in nuts or nut butter, can help provide a sustained energy source.
Incorporating Fiber-Rich Foods

Incorporating fiber-rich foods into the diet is a valuable strategy for hypoglycemia treatment, particularly for individuals with diabetes. Fiber plays a crucial role in regulating blood sugar levels by slowing down the absorption of glucose and promoting overall metabolic health. Here are key points highlighting the importance of incorporating fiber-rich foods in the context of hypoglycemia treatment:
Role of Fiber in Blood Sugar Regulation:
- Slow Absorption of Glucose: Dietary fiber, both soluble and insoluble, slows down the absorption of glucose from the digestive tract. This results in a more gradual and steady release of glucose into the bloodstream.
- Improved Insulin Sensitivity: Regular consumption of fiber has been associated with improved insulin sensitivity. This can contribute to more effective glucose uptake by cells, reducing the risk of hypoglycemia.
Fiber-Rich Food Choices:
- Whole Grains: Opt for whole grains such as brown rice, quinoa, oats, and whole wheat bread. These grains contain bran and germ, which are rich in fiber, vitamins, and minerals.
- Legumes: Beans, lentils, and chickpeas are excellent sources of fiber and plant-based protein. They provide a sustained release of energy without causing rapid spikes in blood sugar.
- Vegetables: Incorporate a variety of non-starchy vegetables into meals, such as leafy greens, broccoli, cauliflower, and bell peppers. These vegetables are low in calories and high in fiber.
- Fruits: Choose whole fruits, which contain fiber along with essential vitamins and minerals. Berries, apples, pears, and citrus fruits are good options.
Hypoglycemia Treatment Guidelines
Hypoglycemia treatment guidelines are essential for individuals, especially those with diabetes, to effectively manage low blood sugar levels. Here are key points outlining general hypoglycemia treatment guidelines:
- Recognition of Symptoms: Individuals should be educated on the early signs and symptoms of hypoglycemia, including shakiness, sweating, irritability, confusion, and dizziness. Recognition is the first step in prompt treatment.
- Blood Sugar Monitoring: Regular monitoring of blood sugar levels is critical for individuals at risk of hypoglycemia. This helps in identifying low blood sugar early and making informed treatment decisions.
- 15-15 Rule: The “15-15 rule” is a common guideline where individuals are advised to consume approximately 15 grams of fast-acting carbohydrates, wait for about 15 minutes, and then recheck blood sugar levels. If levels remain low, another 15 grams of carbohydrates may be consumed.
- Emergency Contacts: Individuals at risk of hypoglycemia should have emergency contacts readily available, and family members, friends, or coworkers should be informed about the appropriate actions to take in case of a severe episode.
- Medical Alert Identification: Wearing a medical alert bracelet or necklace indicating a history of diabetes and the risk of hypoglycemia is important, especially if the individual is unable to communicate during an episode.
- Post-Treatment Monitoring: After consuming carbohydrates, individuals should monitor their blood sugar levels to ensure they rise to a safe range. Repeating the 15-15 rule if necessary is important to prevent recurrence.
Conclusion
In conclusion, effective hypoglycemia treatment involves prompt recognition of symptoms, immediate carbohydrate intake, and regular blood sugar monitoring.
With a focus on self-awareness, proactive measures, and regular adjustments, individuals can navigate hypoglycemia, empowering them to lead fulfilling lives while effectively managing their blood sugar levels.
Do you want to get rid of diabetes? Join our online diabetes treatment program and reverse Diabetes naturally through lifestyle changes such as a Personalized Diet plan, Exercise, Yoga, dieticians, and health coaches.

