Type 2 diabetes, a chronic condition characterized by insulin resistance and elevated blood sugar levels, affects millions of people worldwide. As researchers and healthcare professionals strive to find effective treatments, a range of drugs has emerged to manage and control this condition. This blog aims to provide a detailed overview of the drugs used for Type 2 diabetes, exploring their mechanisms of action, benefits, and potential side effects.
Contents
- 1 What is Type 2 Diabetes?
- 2 Is It Safe To Use Drugs for Type 2 Diabetes?
- 3 List of Drugs for Type 2 Diabetes
- 3.1 Metformin
- 3.2 Sulfonylureas (e.g., Glipizide, Glyburide)
- 3.3 Thiazolidinediones (TZDs) – Pioglitazone, Rosiglitazone
- 3.4 Dipeptidyl Peptidase-4 (DPP-4) Inhibitors (e.g., Sitagliptin, Saxagliptin)
- 3.5 GLP-1 Receptor Agonists (e.g., Exenatide, Liraglutide)
- 3.6 SGLT-2 Inhibitors (e.g., Canagliflozin, Dapagliflozin)
- 3.7 Insulin Therapy
- 4 Conclusion
What is Type 2 Diabetes?

Type 2 diabetes is a chronic metabolic disorder characterized by insulin resistance and impaired insulin secretion. Insulin is a hormone produced by the pancreas that plays a key role in regulating blood sugar (glucose) levels. In individuals with Type 2 diabetes, the body either doesn’t use insulin properly (insulin resistance) or doesn’t produce enough insulin to maintain normal glucose levels.
Insulin resistance occurs when the body’s cells, particularly muscle, liver, and fat cells, become less responsive to the effects of insulin. As a result, glucose is not efficiently transported into these cells, leading to elevated blood sugar levels. To compensate for this, the pancreas produces more insulin, but over time, the beta cells in the pancreas may become exhausted and unable to keep up with the increased demand.
Several factors contribute to the development of Type 2 diabetes, including:
- Genetics: Family history and genetics can play a role in the risk of developing Type 2 diabetes.
- Lifestyle Factors: Poor diet, lack of physical activity, and obesity are significant contributors to the development of insulin resistance and Type 2 diabetes.
- Age: The risk of Type 2 diabetes increases with age, especially after the age of 45.
- Ethnicity: Certain ethnic groups, including African Americans, Hispanic/Latino Americans, Native Americans, and Asian Americans, have a higher risk of developing Type 2 diabetes.
- Medical Conditions: Conditions such as metabolic syndrome, polycystic ovary syndrome (PCOS), and cardiovascular disease are associated with an increased risk of Type 2 diabetes.
Is It Safe To Use Drugs for Type 2 Diabetes?
The use of drugs for Type 2 diabetes is generally safe when prescribed and monitored by healthcare professionals. These medications play a crucial role in managing blood sugar levels and preventing complications associated with diabetes. It’s important to emphasize that the safety and appropriateness of specific medications can vary from person to person, and treatment decisions should be made in consultation with healthcare providers. Here are some key points to consider:
- Individualized Treatment Plans: Healthcare professionals tailor treatment plans based on individual needs, health status, and other factors. The choice of medications, dosage, and treatment goals may vary from person to person.
- Potential Side Effects: Different diabetes medications can have varying side effects. For example, some medications may cause gastrointestinal issues, weight gain, or an increased risk of hypoglycemia (low blood sugar). Understanding potential side effects and discussing them with healthcare providers is important.
- Monitoring and Adjustments: Regular monitoring of blood sugar levels and periodic check-ups with healthcare providers are essential. This allows for adjustments in treatment plans as needed to ensure optimal control of diabetes while minimizing side effects.
- Long-Term Benefits: Effective diabetes management, including the use of medications, can lead to improved long-term outcomes and a reduced risk of complications. Medications help control blood sugar levels and contribute to overall health and well-being.
- Risk-Benefit Analysis: Healthcare providers consider the potential benefits of diabetes medications in controlling blood sugar levels and preventing complications against the potential risks and side effects. The goal is to achieve a balance that optimizes the individual’s health.
- Patient Education: Individuals with Type 2 diabetes must be well-informed about their condition, treatment options, and the importance of adherence to prescribed medications. Patient education empowers individuals to actively participate in their healthcare.
List of Drugs for Type 2 Diabetes
Here is a list of common drugs used for the management of Type 2 diabetes:
Metformin

Description: Metformin stands as the cornerstone in the pharmacological management of Type 2 diabetes, often serving as the initial drug prescribed. Belonging to the biguanide class, Metformin exerts its effects by primarily targeting the liver. It inhibits hepatic gluconeogenesis, reduces the production of glucose in the liver, and enhances insulin sensitivity in peripheral tissues, promoting the uptake of glucose. This dual action results in improved glycemic control without causing excessive insulin release, making Metformin an attractive option for many patients.
One of the notable advantages of Metformin is its long-standing track record of safety and efficacy. It has been utilized for decades, proving its effectiveness in lowering blood sugar levels. Additionally, Metformin is renowned for its affordability, making it a cost-effective choice for many individuals with Type 2 diabetes. The medication’s low risk of hypoglycemia, a condition characterized by dangerously low blood sugar levels, further contributes to its popularity.
However, it’s essential to note that Metformin is not without potential side effects. Gastrointestinal issues, such as nausea and diarrhea, may occur, particularly at the initiation of treatment. These side effects are generally transient and diminish over time. Furthermore, Metformin may be contraindicated in individuals with certain kidney conditions, necessitating careful consideration and monitoring by healthcare professionals.
Sulfonylureas (e.g., Glipizide, Glyburide)
Description: Sulfonylureas constitute a class of oral antidiabetic medications that have been used extensively in the management of Type 2 diabetes. Examples include Glipizide and Glyburide. The primary mechanism of action involves stimulating insulin release from the beta cells of the pancreas. By enhancing insulin secretion, sulfonylureas facilitate the uptake of glucose by cells, thereby reducing blood sugar levels.
While sulfonylureas are effective in lowering blood glucose, their use is associated with a higher risk of hypoglycemia compared to some newer antidiabetic medications. Hypoglycemia can manifest as symptoms such as shakiness, sweating, and confusion and, in severe cases, can lead to loss of consciousness. Therefore, careful monitoring of blood glucose levels and individualizing the dosage is crucial to minimize this risk.
Sulfonylureas are often considered when Metformin alone does not provide adequate glycemic control. However, healthcare providers must assess the patient’s overall health, including kidney function, before prescribing sulfonylureas. In certain situations, the potential for weight gain associated with these medications may also be a consideration.
Thiazolidinediones (TZDs) – Pioglitazone, Rosiglitazone
Description: Thiazolidinediones, commonly known as TZDs, represent a class of oral antidiabetic medications with a mechanism of action centered around improving insulin sensitivity in peripheral tissues. Pioglitazone and Rosiglitazone are two examples. These drugs activate peroxisome proliferator-activated receptors (PPARs), specifically PPAR-gamma, leading to enhanced insulin action.
Despite their effectiveness in addressing insulin resistance, TZDs have notable considerations. Weight gain is a common side effect, and individuals with a history of heart failure may need to exercise caution, as TZDs are associated with an increased risk of heart failure. Additionally, the potential for an increased risk of bone fractures has been observed, especially in postmenopausal women.
TZDs are often utilized when other oral antidiabetic medications have not achieved the desired glycemic control. Close monitoring of cardiovascular health and regular check-ups with healthcare providers is imperative to ensure the safety and appropriateness of TZD therapy.
Dipeptidyl Peptidase-4 (DPP-4) Inhibitors (e.g., Sitagliptin, Saxagliptin)
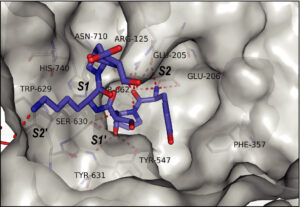
Description: Dipeptidyl peptidase-4 (DPP-4) inhibitors constitute a relatively newer class of oral antidiabetic medications designed to enhance glycemic control in Type 2 diabetes. Examples include Sitagliptin and Saxagliptin. The primary mechanism of action involves inhibiting the DPP-4 enzyme, which is responsible for the degradation of incretin hormones, particularly glucagon-like peptide-1 (GLP-1).
By inhibiting DPP-4, these medications increase the levels of active GLP-1. The enhanced GLP-1 levels stimulate insulin secretion while inhibiting glucagon release, resulting in improved glucose regulation. DPP-4 inhibitors are known for their favorable safety profile, with a lower risk of hypoglycemia compared to some other antidiabetic medications.
DPP-4 inhibitors are often considered in combination therapy or when Metformin alone is insufficient to achieve glycemic targets. However, individuals with impaired kidney function should use these medications cautiously, as some may require dosage adjustments based on renal function.
GLP-1 Receptor Agonists (e.g., Exenatide, Liraglutide)
Description: Glucagon-like peptide-1 (GLP-1) receptor agonists represent injectable medications used in the management of Type 2 diabetes. Examples include Exenatide and Liraglutide. These drugs mimic the effects of endogenous GLP-1, a hormone that enhances insulin secretion, reduces glucagon production, and slows gastric emptying.
One of the notable benefits of GLP-1 receptor agonists is their association with weight loss. This makes them particularly attractive for individuals with Type 2 diabetes who may also struggle with obesity. Additionally, the use of GLP-1 receptor agonists has been linked to cardiovascular benefits, making them a valuable option for those with underlying cardiovascular risk factors.
Given their injectable nature, patient education regarding administration techniques is crucial. Common side effects include gastrointestinal symptoms, such as nausea, which may decrease over time. As with any medication, careful consideration of individual health status and preferences is necessary when prescribing GLP-1 receptor agonists.
SGLT-2 Inhibitors (e.g., Canagliflozin, Dapagliflozin)
Description: Sodium-glucose co-transporter-2 (SGLT-2) inhibitors represent a relatively recent addition to the armamentarium of antidiabetic medications. Examples include Canagliflozin and Dapagliflozin. The unique mechanism of action of SGLT-2 inhibitors involves blocking the reabsorption of glucose in the kidneys, leading to increased glucose excretion in urine.
This mechanism results in both glycemic control and additional cardiovascular benefits. SGLT-2 inhibitors have shown efficacy in reducing the risk of cardiovascular events and heart failure in individuals with Type 2 diabetes. Additionally, they are associated with a mild diuretic effect, contributing to blood pressure reduction.
Common side effects of SGLT-2 inhibitors include an increased risk of urinary tract infections and genital mycotic infections. Patients are often advised to maintain good hydration and proper hygiene to mitigate these risks. As with other antidiabetic medications, close monitoring by healthcare providers is essential to ensure safety and efficacy.
Insulin Therapy

Description: Insulin remains a fundamental component in the management of Type 2 diabetes, especially as the disease progresses. Various types of insulin cater to different physiological needs. Rapid-acting insulin addresses postprandial glucose spikes, short-acting insulin covers meals, intermediate-acting insulin provides basal coverage, and long-acting insulin offers a sustained release over an extended period.
Insulin therapy is often considered when lifestyle modifications and oral medications alone are insufficient to achieve glycemic targets. It allows for precise control over blood sugar levels by supplementing or replacing the body’s natural insulin production. The choice of insulin regimen depends on factors such as the individual’s lifestyle, eating patterns, and blood glucose patterns throughout the day.
While insulin is highly effective in controlling blood sugar levels, its use requires careful monitoring and adherence to dosage recommendations. Additionally, patients need education on proper injection techniques, insulin storage, and blood glucose monitoring to optimize glycemic control.
Conclusion
The landscape of Type 2 diabetes treatment has evolved significantly, providing healthcare providers and patients with a range of options to manage this chronic condition. While drug therapies play a crucial role, lifestyle modifications, including a healthy diet and regular exercise, remain fundamental in diabetes management. As research continues, we can anticipate further advancements and innovations in the quest for more effective and personalized treatments for Type 2 diabetes. Always consult with healthcare professionals to determine the most appropriate treatment plan based on individual needs and circumstances.
Do you want to get rid of diabetes? Join our online diabetes treatment program and reverse Diabetes naturally through lifestyle changes such as a Personalized Diet plan, Exercise, Yoga, dieticians, and health coaches.

