Type 2 diabetes is a chronic metabolic disorder characterized by elevated blood sugar levels due to insulin resistance and relative insulin deficiency. It affects millions worldwide and requires lifelong management to prevent complications. While lifestyle modifications like diet and exercise play a crucial role, medication often becomes necessary to control blood sugar levels effectively. Among the various treatment options available, oral medications form the cornerstone of type 2 diabetes management for many individuals. Keep reading this blog for more information on oral medication for Type 2 diabetes.
Contents
- 1 Can Oral Medication Treat Type 2 Diabetes?
- 2 Types of Oral Medications for Type 2 Diabetes
- 3 Choosing the Right Oral Medication for Type 2 Diabetes
- 3.1 Assessing Medical History and Comorbidities
- 3.2 Evaluating Disease Severity and Glycemic Control
- 3.3 Considering Lifestyle Factors
- 3.4 Understanding Mechanism of Action and Side Effects
- 3.5 Considering Cardiovascular and Renal Health
- 3.6 Individualizing Treatment Plans
- 3.7 Educating and Empowering Patients
- 4 How To Take Oral Mediation for Type 2 Diabetes?
- 5 Conclusion
Can Oral Medication Treat Type 2 Diabetes?

Overall, oral medications are highly effective in managing type 2 diabetes, particularly when used as part of a comprehensive treatment approach that includes lifestyle modifications and regular monitoring. The effectiveness of oral medications can vary depending on individual factors such as age, disease duration, severity of insulin resistance, presence of comorbidities, and medication adherence.
Studies have consistently shown that oral medications, either used alone or in combination, can significantly reduce HbA1c levels (a measure of long-term blood sugar control) and lower the risk of diabetes-related complications. However, it’s essential to recognize that no single medication is universally effective for all individuals with type 2 diabetes, and treatment may need to be tailored based on individual needs and responses.
Here are some benefits of it:
Blood Sugar Control
Oral medications help lower blood sugar levels by various mechanisms, including reducing glucose production in the liver, increasing insulin secretion, improving insulin sensitivity, and delaying carbohydrate absorption in the gut. By regulating blood sugar levels, these medications help prevent hyperglycemia, which is associated with long-term complications such as cardiovascular disease, kidney disease, neuropathy, and retinopathy.
Ease of Administration
Unlike insulin therapy, which often requires injections, oral medications are taken in pill or tablet form, making them more convenient and less invasive for many individuals. This ease of administration can improve medication adherence and overall treatment compliance, leading to better glycemic control and reduced risk of complications.
Delaying Disease Progression
Effective management of type 2 diabetes with oral medications can slow down the progression of the disease and preserve beta-cell function over time. By maintaining adequate insulin production and sensitivity, these medications help prevent the need for insulin therapy and delay the onset of complications associated with advanced diabetes.
Cardiovascular Protection
Some oral medications, such as sodium-glucose cotransporter-2 (SGLT2) inhibitors and glucagon-like peptide-1 (GLP-1) receptor agonists, have demonstrated cardiovascular benefits beyond glycemic control. These medications reduce the risk of major adverse cardiovascular events, including heart attack, stroke, and cardiovascular death, making them valuable additions to the treatment regimen for individuals with type 2 diabetes and established cardiovascular disease or high cardiovascular risk.
Weight Management
Certain oral medications, such as metformin and GLP-1 receptor agonists, have been associated with weight loss or weight neutrality, making them suitable choices for individuals who need to manage their weight as part of their diabetes treatment plan. Weight loss can improve insulin sensitivity, reduce insulin resistance, and lower cardiovascular risk factors, thereby contributing to better overall health outcomes.
Types of Oral Medications for Type 2 Diabetes
Here are the main types of oral medications used for the management of type 2 diabetes:
Biguanides

Biguanides, such as metformin, are among the most commonly prescribed oral medications for type 2 diabetes. Metformin works by reducing glucose production in the liver and improving insulin sensitivity in peripheral tissues. It does not increase insulin secretion from the pancreas, making it less likely to cause hypoglycemia. Additionally, metformin has been shown to have beneficial effects on weight loss and cardiovascular health.
Metformin is typically recommended as first-line therapy for type 2 diabetes due to its efficacy, safety profile, and relatively low cost. It is available in various formulations, including immediate-release and extended-release tablets. Common side effects of metformin may include gastrointestinal symptoms such as nausea, diarrhea, and abdominal discomfort, which can often be minimized by starting with a low dose and gradually increasing it over time.
Sulfonylureas
Sulfonylureas stimulate insulin secretion from the pancreatic beta cells, thereby lowering blood sugar levels. Examples of sulfonylureas include glyburide, glipizide, and glimepiride. These medications are typically taken once or twice daily before meals.
While sulfonylureas are effective at lowering blood glucose levels, they are associated with a higher risk of hypoglycemia compared to other oral medications. They may also cause weight gain due to increased insulin secretion. Therefore, sulfonylureas are often used as second-line therapy or in combination with other medications for individuals who fail to achieve adequate glycemic control with lifestyle modifications and metformin.
Dipeptidyl Peptidase-4 (DPP-4) Inhibitors
DPP-4 inhibitors, such as sitagliptin, saxagliptin, and linagliptin, work by inhibiting the enzyme DPP-4, which degrades incretin hormones. By prolonging the action of incretins, DPP-4 inhibitors stimulate insulin secretion and inhibit glucagon release, resulting in lower blood sugar levels.
One of the main advantages of DPP-4 inhibitors is their low risk of hypoglycemia. They are generally well-tolerated and can be used alone or in combination with other oral medications for type 2 diabetes. Common side effects may include upper respiratory tract infections, headaches, and nasopharyngitis.
Sodium-Glucose Cotransporter-2 (SGLT2) Inhibitors
SGLT2 inhibitors, such as canagliflozin, dapagliflozin, and empagliflozin, work by blocking the reabsorption of glucose in the kidneys, leading to increased urinary glucose excretion and lower blood sugar levels. In addition to their glucose-lowering effects, SGLT2 inhibitors have been shown to reduce the risk of cardiovascular events and kidney disease progression in individuals with type 2 diabetes and established cardiovascular disease or high cardiovascular risk.
Common side effects of SGLT2 inhibitors include genital yeast infections, urinary tract infections, and increased urination. They may also be associated with a small increase in the risk of diabetic ketoacidosis, particularly in individuals with type 1 diabetes or those with risk factors such as dehydration or acute illness.
Thiazolidinediones (TZDs)
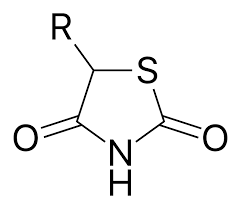
TZDs, such as pioglitazone and rosiglitazone, improve insulin sensitivity in peripheral tissues by activating peroxisome proliferator-activated receptor gamma (PPAR-γ). They reduce insulin resistance and lower blood sugar levels, particularly in individuals with insulin resistance or metabolic syndrome.
One of the main benefits of TZDs is their effect on insulin sensitivity, which can lead to improvements in glycemic control and lipid profiles. However, TZDs are associated with an increased risk of weight gain, fluid retention, and bone fractures. Therefore, they are typically used with caution and may not be suitable for individuals with heart failure or a history of bladder cancer.
Alpha-Glucosidase Inhibitors
Alpha-glucosidase inhibitors, such as acarbose and miglitol, delay the digestion and absorption of carbohydrates in the small intestine, resulting in a slower rise in blood sugar levels after meals. They are often used as adjunctive therapy to other oral medications or insulin for individuals who have difficulty controlling postprandial glucose levels.
Alpha-glucosidase inhibitors are associated with gastrointestinal side effects such as flatulence, diarrhea, and abdominal discomfort, which can limit their tolerability and adherence. They are typically taken with the first bite of each main meal to maximize their effectiveness in controlling postprandial glucose excursions.
Glucagon-Like Peptide-1 (GLP-1) Receptor Agonists
GLP-1 receptor agonists, such as exenatide, liraglutide, and dulaglutide, mimic the action of the endogenous incretin hormone GLP-1. They stimulate insulin secretion in a glucose-dependent manner, suppress glucagon secretion, slow gastric emptying, and promote satiety, leading to improved glycemic control and weight loss.
GLP-1 receptor agonists are typically administered by subcutaneous injection once daily or once weekly. They are associated with gastrointestinal side effects such as nausea, vomiting, and diarrhea, particularly when initiated at higher doses.
However, these side effects often diminish over time with continued use. GLP-1 receptor agonists have also been shown to have cardiovascular benefits, including reductions in major adverse cardiovascular events, making them valuable therapeutic options for individuals with type 2 diabetes and established cardiovascular disease or high cardiovascular risk.
Choosing the Right Oral Medication for Type 2 Diabetes

Choosing the right oral medication for type 2 diabetes requires consideration of several factors, including the individual’s medical history, disease severity, comorbidities, lifestyle, preferences, and cost. Here are some key steps to guide the selection process:
Assessing Medical History and Comorbidities
- Review the patient’s medical history, including any previous treatment for diabetes and other chronic conditions.
- Consider comorbidities such as cardiovascular disease, renal impairment, liver disease, and gastrointestinal disorders, as certain oral medications may be contraindicated or require dose adjustments in these conditions.
Evaluating Disease Severity and Glycemic Control
- Assess the severity of diabetes based on factors such as HbA1c levels, fasting and postprandial glucose levels, and the presence of symptoms.
- Determine the target HbA1c level based on individualized goals and guidelines from professional organizations.
Considering Lifestyle Factors
- Take into account the patient’s lifestyle, including dietary habits, physical activity level, and ability to adhere to medication regimens.
- Discuss the importance of lifestyle modifications such as diet and exercise in diabetes management and how oral medications can complement these efforts.
Understanding Mechanism of Action and Side Effects
- Educate the patient about the different classes of oral medications available for type 2 diabetes and their mechanisms of action.
- Discuss the potential side effects and safety profiles of each medication class, including the risk of hypoglycemia, weight gain, gastrointestinal symptoms, and other adverse effects.
Considering Cardiovascular and Renal Health
- Consider the patient’s cardiovascular risk profile and the potential cardiovascular benefits of certain oral medications, such as SGLT2 inhibitors and GLP-1 receptor agonists.
- Assess renal function and choose medications that are safe and appropriate for individuals with kidney disease, as some medications may require dose adjustments or should be avoided in this population.
Individualizing Treatment Plans
- Tailor treatment plans to meet the patient’s specific needs and preferences, taking into account their preferences for oral medications, dosing frequency, route of administration, and potential cost considerations.
- Consider the possibility of combination therapy with multiple oral medications or with insulin to achieve optimal glycemic control, particularly in individuals with higher HbA1c levels or more advanced diseases.
Educating and Empowering Patients
- Educate patients about the importance of medication adherence, regular monitoring of blood glucose levels, and self-management strategies for diabetes control.
- Empower patients to actively participate in decision-making regarding their diabetes treatment, including discussing concerns, asking questions, and setting realistic goals for glycemic control and overall health.
How To Take Oral Mediation for Type 2 Diabetes?

Taking oral medication for type 2 diabetes requires careful attention to ensure safety and effectiveness. Here are some precautions to consider:
Follow the Prescribed Dosage and Schedule
- Take the medication exactly as prescribed by your healthcare provider, including the correct dosage and timing.
- Do not adjust the dosage or frequency without consulting your healthcare provider, as this can affect blood sugar control and increase the risk of complications.
Monitor Blood Glucose Levels
- Regularly monitor your blood glucose levels as directed by your healthcare provider, especially when starting a new medication or making changes to your treatment regimen.
- Keep a record of your blood sugar readings and share them with your healthcare provider during follow-up visits.
Be Aware of Side Effects
- Familiarize yourself with the potential side effects of your medication and know when to seek medical attention.
- Common side effects of oral diabetes medications may include gastrointestinal symptoms, such as nausea, diarrhea, and abdominal discomfort, as well as hypoglycemia (low blood sugar) and allergic reactions.
Stay Hydrated
- Some medications, such as SGLT2 inhibitors, may increase the risk of dehydration and electrolyte imbalances.
- Drink plenty of water and stay hydrated, especially during hot weather or when engaging in physical activity, to help prevent dehydration.
Monitor Kidney Function
- Certain oral medications, particularly those in the SGLT2 inhibitor class, may affect kidney function.
- Monitor your kidney function regularly through blood tests as recommended by your healthcare provider, and report any signs of kidney problems, such as changes in urine output or swelling in the legs or feet.
Take Precautions During Illness
- During illness or times of stress, blood sugar levels may fluctuate unpredictably.
- Continue taking your medication as prescribed, and monitor your blood sugar levels more frequently.
- Stay hydrated, eat small, frequent meals if you have difficulty eating, and contact your healthcare provider if you experience persistent hyperglycemia or other concerning symptoms.
Avoid Alcohol Abuse
- Alcohol consumption can affect blood sugar levels and interact with certain diabetes medications.
- Limit alcohol intake to moderate amounts as recommended by your healthcare provider, and avoid excessive drinking, which can lead to poor blood sugar control and other health complications.
Maintain a Healthy Lifestyle
- Adopt healthy lifestyle habits, including eating a balanced diet, engaging in regular physical activity, getting an adequate amount of sleep, and managing stress.
- These lifestyle modifications can complement the effects of oral medications in controlling blood sugar levels and improving overall health outcomes.
Communicate with Your Healthcare Provider
- Keep open communication with your healthcare provider regarding any concerns or changes in your health status.
- Inform your healthcare provider about all medications, supplements, and over-the-counter drugs you are taking, as they may interact with your diabetes medication.
Conclusion
Oral medications play a crucial role in the management of type 2 diabetes by lowering blood sugar levels and reducing the risk of complications. Understanding the different classes of oral medications, their mechanisms of action, and factors influencing treatment selection is essential for healthcare providers and individuals with type 2 diabetes alike. With proper medication management, lifestyle modifications, and regular monitoring, individuals with type 2 diabetes can effectively control their condition and lead healthy, fulfilling lives.

