In the modern era, where sedentary lifestyles and processed foods have become the norm, the prevalence of diabetes and other metabolic disorders has surged. As a result, the need for effective sugar control has never been more critical. While lifestyle modifications such as diet and exercise play a pivotal role, sugar control medicines have become indispensable in managing blood glucose levels. In this blog, we will delve into the intricacies of sugar control medicines, exploring their types, mechanisms, and considerations for use.
Contents
- 1 What Does “Sugar Control” Mean?
- 2 List of Sugar Control Medicines
- 2.1 Metformin
- 2.2 Insulin
- 2.3 Sulfonylureas (e.g., Glipizide, Glibenclamide)
- 2.4 GLP-1 Receptor Agonists (e.g., Exenatide, Liraglutide)
- 2.5 SGLT2 Inhibitors (e.g., Canagliflozin, Dapagliflozin)
- 2.6 DPP-4 Inhibitors (e.g., Sitagliptin, Saxagliptin):
- 2.7 Alpha-glucosidase Inhibitors (e.g., Acarbose, Miglitol)
- 2.8 Meglitinides (e.g., Repaglinide, Nateglinide)
- 2.9 Thiazolidinediones (e.g., Pioglitazone, Rosiglitazone)
- 2.10 Amylinomimetics (e.g., Pramlintide)
- 3 Steps After Taking Sugar Control Medicines
- 4 Conclusion
What Does “Sugar Control” Mean?
“Sugar control” refers to the regulation and maintenance of blood sugar levels within a specific and healthy range. Blood sugar, or blood glucose, is a type of sugar that is present in the bloodstream and serves as the primary source of energy for cells. The body tightly regulates blood sugar levels to ensure a stable and optimal environment for various physiological functions.
In the context of health, particularly in managing conditions such as diabetes, sugar control becomes crucial. Diabetes is a chronic condition characterized by elevated levels of blood sugar, either due to insufficient insulin production (Type 1 diabetes) or ineffective use of insulin by the body (Type 2 diabetes). In individuals without diabetes, the pancreas releases insulin to help cells absorb glucose from the bloodstream, thus maintaining blood sugar levels within a normal range.
Sugar control involves measures and interventions aimed at preventing high or low blood sugar levels, especially in individuals with diabetes. The goal is to keep blood glucose levels within a target range to prevent complications and promote overall well-being. This can be achieved through a combination of lifestyle modifications, such as a balanced diet and regular exercise, as well as, in some cases, the use of medications or insulin.
List of Sugar Control Medicines
In the realm of diabetes management, sugar control medicines play a pivotal role in regulating blood glucose levels. From oral medications to injectables, this list provides concise overviews of various classes of sugar control medicines and their mechanisms of action:
Metformin

- Overview: Metformin is a first-line medication for managing Type 2 diabetes. It belongs to the biguanide class and works by reducing glucose production in the liver and improving insulin sensitivity in the body’s tissues.
- Mechanism of Action: Metformin primarily decreases the amount of glucose produced by the liver, thus lowering blood sugar levels. It also enhances the body’s response to insulin, allowing cells to take up glucose more efficiently.
- Considerations: Metformin is often prescribed as an initial therapy for Type 2 diabetes and is known for its safety profile. Side effects may include gastrointestinal issues, and it is usually taken with meals to minimize these effects.
Insulin
- Overview: Insulin is a hormone naturally produced by the pancreas, and for individuals with diabetes, it may need to be administered through injections. There are various types of insulin with different onset and duration profiles.
- Mechanism of Action: Insulin facilitates the uptake of glucose by cells, reducing blood sugar levels. The different types of insulin are categorized based on their speed of onset and duration of action, allowing for flexibility in managing blood glucose levels.
- Considerations: Insulin therapy is crucial for individuals with Type 1 diabetes and may also be prescribed for those with Type 2 diabetes when oral medications are not sufficient. The specific type and regimen depend on individual needs and lifestyle.
Sulfonylureas (e.g., Glipizide, Glibenclamide)
- Overview: Sulfonylureas are a class of oral antidiabetic drugs that stimulate insulin secretion from the pancreas.
- Mechanism of Action: These drugs enhance insulin release, helping to lower blood sugar levels by promoting the uptake of glucose by cells.
- Considerations: While effective, sulfonylureas may cause hypoglycemia (low blood sugar) as a side effect. They are usually taken before meals to coincide with food-induced rises in blood sugar.
GLP-1 Receptor Agonists (e.g., Exenatide, Liraglutide)
- Overview: GLP-1 receptor agonists are injectable medications that mimic the action of the naturally occurring hormone GLP-1, which stimulates insulin release and reduces glucose production.
- Mechanism of Action: These drugs enhance insulin secretion, slow gastric emptying, and reduce appetite, contributing to improved blood sugar control.
- Considerations: GLP-1 receptor agonists are often used as adjunctive therapy for Type 2 diabetes, providing a once-weekly injection option for some formulations.
SGLT2 Inhibitors (e.g., Canagliflozin, Dapagliflozin)
- Overview: Sodium-glucose co-transporter-2 (SGLT2) inhibitors are oral medications that reduce glucose reabsorption by the kidneys, leading to increased glucose excretion in urine.
- Mechanism of Action: By promoting the elimination of excess glucose through urine, SGLT2 inhibitors help lower blood sugar levels.
- Considerations: These medications may be associated with an increased risk of urinary tract infections and dehydration. They are often used in conjunction with other antidiabetic drugs.
DPP-4 Inhibitors (e.g., Sitagliptin, Saxagliptin):
- Overview: DPP-4 inhibitors are oral medications that target dipeptidyl peptidase-4, an enzyme that breaks down incretin hormones. Incretins help regulate blood sugar by increasing insulin release and decreasing glucagon production.
- Mechanism of Action: DPP-4 inhibitors prolong the action of incretins, leading to increased insulin release and reduced glucose production.
- Considerations: These medications are generally well-tolerated and are used as part of the management of Type 2 diabetes.
Alpha-glucosidase Inhibitors (e.g., Acarbose, Miglitol)
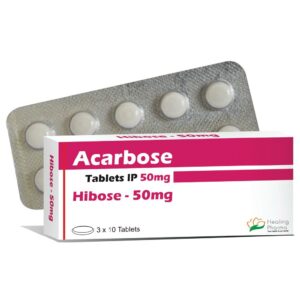
- Overview: Alpha-glucosidase inhibitors are oral medications that slow down the digestion of carbohydrates in the intestines, resulting in a gradual rise in blood sugar levels after meals.
- Mechanism of Action: These inhibitors delay the absorption of glucose from the gastrointestinal tract, helping to control postprandial (after-meal) blood sugar levels.
- Considerations: Side effects may include gastrointestinal discomfort, and these medications are often taken with the first bite of each main meal.
Meglitinides (e.g., Repaglinide, Nateglinide)
- Overview: Meglitinides are another class of oral antidiabetic drugs that stimulate insulin release from the pancreas, similar to sulfonylureas.
- Mechanism of Action: These drugs act quickly to enhance insulin secretion, especially in response to meals, contributing to improved blood sugar control.
- Considerations: Meglitinides are taken before meals and are suitable for individuals who have irregular meal schedules.
Thiazolidinediones (e.g., Pioglitazone, Rosiglitazone)
- Overview: Thiazolidinediones, also known as TZDs, are oral medications that improve insulin sensitivity in peripheral tissues like muscles and adipose tissue.
- Mechanism of Action: TZDs activate peroxisome proliferator-activated receptor-gamma (PPAR-gamma), leading to enhanced insulin action and reduced glucose production.
- Considerations: These medications may be associated with weight gain and an increased risk of heart-related issues. They are often used in combination with other antidiabetic drugs.
Amylinomimetics (e.g., Pramlintide)
- Overview: Pramlintide is an injectable medication that mimics the action of amylin, a hormone co-secreted with insulin that regulates blood sugar by slowing gastric emptying and reducing glucagon release.
- Mechanism of Action: By slowing down the movement of food through the stomach, pramlintide helps control postprandial blood sugar levels.
- Considerations: It is typically used in conjunction with insulin for individuals with Type 1 or Type 2 diabetes.
These additional medications offer a broader understanding of the diverse pharmacological approaches available for sugar control.
Steps After Taking Sugar Control Medicines

After taking sugar control medicines, there are several important steps to follow to ensure optimal effectiveness and safety. Here is a comprehensive guide on what to do after taking your sugar control medications:
- Observe for Immediate Effects: Some medications may have immediate effects on blood sugar levels. Pay attention to any signs or symptoms, such as dizziness, weakness, or vision changes, which could indicate hypoglycemia (low blood sugar). If you experience these symptoms, have a source of fast-acting glucose on hand, such as glucose tablets or juice, as recommended by your healthcare provider.
- Timing of Meals: If your medication is supposed to be taken with or before meals, ensure that you eat within the recommended time frame. This helps synchronize the action of the medication with the digestion of food, optimizing blood sugar control.
- Maintain a Regular Eating Schedule: Consistency in meal timing can contribute to stable blood sugar levels. Try to maintain a regular eating schedule with balanced meals and snacks throughout the day.
- Stay Hydrated: Adequate hydration is essential for overall health, especially if you are taking certain types of sugar control medications like SGLT2 inhibitors. Drink water regularly to stay hydrated, unless otherwise advised by your healthcare provider.
- Physical Activity: Engage in regular physical activity as recommended by your healthcare team. Exercise can help improve insulin sensitivity and contribute to better sugar control. However, be mindful of the timing of exercise with your medication to prevent hypoglycemia.
- Blood Sugar Monitoring: Regularly monitor your blood sugar levels, especially if your healthcare provider has recommended routine testing. This helps track the effectiveness of your medication and allows for timely adjustments to your treatment plan.
Conclusion
Sugar control medicines play a vital role in managing diabetes and maintaining healthy blood glucose levels. From insulin to oral antidiabetic drugs, each medication type has its unique mechanisms and considerations. The key lies in developing personalized treatment plans, encompassing medication, diet, and exercise. As research continues to advance, the future promises even more targeted and effective sugar control options. Ultimately, the journey to optimal sugar control is a collaborative effort between healthcare providers and individuals, working hand in hand to achieve and maintain a delicate balance in the intricate dance of blood glucose regulation.
Do you want to get rid of diabetes? Join our online diabetes treatment program and reverse Diabetes naturally through lifestyle changes such as a Personalized Diet plan, Exercise, Yoga, dieticians, and health coaches.

