Managing blood sugar levels is crucial for individuals with diabetes to prevent complications and maintain overall health. A1C, or glycated hemoglobin, is a key indicator of long-term blood sugar control. Medications play a significant role in lowering A1C levels, alongside lifestyle changes such as diet and exercise. In this comprehensive guide, we’ll explore various medications used to lower A1C levels, how they work, their benefits, potential side effects, and other essential considerations.
Contents
What is A1C?
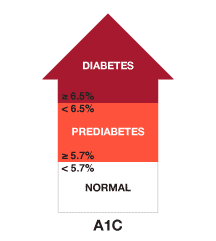
A1C, also known as glycated hemoglobin, is a crucial measure used in managing diabetes. It indicates average blood glucose levels over approximately two to three months. The term “A1C” refers to the attachment of glucose molecules to hemoglobin, the protein found in red blood cells that carries oxygen throughout the body.
When blood sugar levels are elevated over time, glucose molecules can attach themselves to hemoglobin in a process known as glycation. The higher the blood sugar levels, the more glucose attaches to hemoglobin. As red blood cells have a lifespan of about two to three months, measuring the percentage of glycated hemoglobin provides an estimate of average blood glucose levels during that period.
List of Medications to Lower A1C
Lowering A1C levels is a key goal in managing diabetes, as it helps reduce the risk of complications and improves overall health outcomes. Several medications are available to help individuals achieve target A1C levels, and they work through various mechanisms to control blood sugar levels. Here’s an overview of some common medications used to lower A1C:
Metformin
- Metformin is often the first-line medication for type 2 diabetes.
- It belongs to the class of drugs known as biguanides and works primarily by reducing glucose production in the liver and improving insulin sensitivity in muscle cells.
- Metformin may also help lower A1C levels by decreasing glucose absorption from the intestines.
- It is generally well-tolerated but may cause gastrointestinal side effects such as nausea, diarrhea, and abdominal discomfort in some individuals.
Sulfonylureas
- Sulfonylureas stimulate the pancreas to release more insulin, which helps lower blood sugar levels.
- Examples include glyburide, glipizide, and glimepiride.
- Sulfonylureas are effective in lowering A1C levels but may cause weight gain and hypoglycemia (low blood sugar) as potential side effects.
- They are typically used in individuals with type 2 diabetes who cannot achieve target blood sugar levels with lifestyle changes or metformin alone.
DPP-4 Inhibitors (Dipeptidyl Peptidase-4 Inhibitors)
- DPP-4 inhibitors work by increasing insulin secretion and decreasing glucagon production, leading to lower blood sugar levels.
- Examples include sitagliptin, saxagliptin, and linagliptin.
- DPP-4 inhibitors are generally well-tolerated and do not typically cause hypoglycemia as a side effect.
- They are often used as adjunctive therapy in individuals with type 2 diabetes who require additional blood sugar control beyond metformin or sulfonylureas.
GLP-1 Receptor Agonists (Glucagon-Like Peptide-1 Receptor Agonists)

- GLP-1 receptor agonists mimic the action of glucagon-like peptide-1 (GLP-1), which stimulates insulin secretion, slows gastric emptying, and reduces appetite.
- Examples include exenatide, liraglutide, and dulaglutide.
- GLP-1 receptor agonists are associated with weight loss and may also reduce the risk of cardiovascular events.
- They are typically used in individuals with type 2 diabetes who require additional blood sugar control and may be used alone or in combination with other medications.
SGLT2 Inhibitors (Sodium-Glucose Cotransporter-2 Inhibitors)
- SGLT2 inhibitors work by blocking the reabsorption of glucose by the kidneys, leading to increased glucose excretion in the urine.
- Examples include canagliflozin, dapagliflozin, and empagliflozin.
- SGLT2 inhibitors have been shown to reduce A1C levels, lower blood pressure, and decrease the risk of heart failure.
- They are often used in individuals with type 2 diabetes to improve blood sugar control and reduce cardiovascular risk.
Insulin Therapy
- Insulin therapy may be necessary for individuals with type 1 diabetes or those with type 2 diabetes who cannot achieve target A1C levels with oral medications alone.
- Various types of insulin are available, including rapid-acting, short-acting, intermediate-acting, and long-acting formulations.
- Insulin therapy requires careful monitoring of blood sugar levels to prevent hypoglycemia and adjust insulin doses accordingly.
- It may be used alone or in combination with oral medications to achieve target blood sugar levels.
Benefits of Lowering A1C
Lowering A1C levels in individuals with diabetes offers numerous benefits, as it indicates better control of blood sugar levels over time. Here are some key benefits of achieving and maintaining lower A1C levels:
Reduced Risk of Diabetes Complications
- Lowering A1C levels significantly reduces the risk of long-term complications associated with diabetes. These complications include cardiovascular disease (heart disease and stroke), kidney disease, nerve damage (neuropathy), eye damage (retinopathy), and foot problems.
- Improved blood sugar control helps prevent or delay the onset and progression of these complications, leading to better overall health and quality of life.
Cardiovascular Health
- Lowering A1C levels is associated with a decreased risk of cardiovascular events such as heart attacks and strokes. Diabetes is a major risk factor for cardiovascular disease, and tight blood sugar control helps mitigate this risk.
- Certain medications used to lower A1C levels, such as GLP-1 receptor agonists and SGLT2 inhibitors, have been shown to provide additional cardiovascular benefits beyond blood sugar control, including reducing the risk of heart failure and cardiovascular death.
Improved Energy Levels and Well-Being
- Stable blood sugar levels result in more consistent energy levels throughout the day. By keeping blood sugar within target ranges, individuals with diabetes may experience reduced fatigue and improved overall well-being.
- Better blood sugar control can also lead to improved mood and mental health, as fluctuations in blood sugar levels can affect cognitive function and emotional stability.
Delayed Progression of Diabetes
- Lowering A1C levels helps slow the progression of diabetes by preserving beta-cell function (cells in the pancreas that produce insulin) and reducing insulin resistance.
- Early intervention with lifestyle modifications and medications can help individuals with prediabetes or early-stage diabetes delay or prevent the need for more intensive treatment in the future.
Enhanced Quality of Life
- Maintaining lower A1C levels allows individuals with diabetes to lead more active and productive lives. By minimizing the impact of diabetes-related complications, individuals can engage in daily activities, pursue hobbies and interests, and maintain social connections without significant limitations.
- Improved blood sugar control can also reduce the burden of managing diabetes-related symptoms and complications, leading to a better overall quality of life.
Long-Term Health Benefits
- Lowering A1C levels has long-term health benefits, including reduced healthcare costs associated with diabetes-related complications and hospitalizations.
- By effectively managing blood sugar levels, individuals with diabetes can potentially extend their life expectancy and reduce the risk of premature mortality.
Potential Side Effects and Considerations
While medications used to lower A1C levels are generally effective in managing diabetes, they may also be associated with certain side effects and considerations. Individuals need to be aware of these potential risks and discuss them with their healthcare providers. Here are some common side effects and considerations associated with medications to lower A1C:
Hypoglycemia (Low Blood Sugar)
- Hypoglycemia is a potential side effect of many diabetes medications, particularly sulfonylureas and insulin.
- Symptoms of hypoglycemia may include shakiness, dizziness, sweating, confusion, irritability, hunger, and rapid heartbeat.
- Individuals taking medications that can cause hypoglycemia should be educated on how to recognize and treat low blood sugar episodes promptly.
Gastrointestinal Side Effects
- Some diabetes medications, such as metformin and GLP-1 receptor agonists, may cause gastrointestinal side effects such as nausea, diarrhea, vomiting, and abdominal discomfort.
- These side effects are usually mild and may improve over time or with dose adjustments. However, they can sometimes be bothersome and affect medication adherence.
Weight Gain
- Certain diabetes medications, including sulfonylureas and insulin, may lead to weight gain as a side effect.
- Weight gain can pose challenges for individuals trying to manage their diabetes or maintain a healthy weight.
- Healthcare providers may need to monitor weight regularly and adjust treatment plans as needed to minimize weight gain and its impact on overall health.
Allergic Reactions
- Allergic reactions to diabetes medications are rare but possible. Symptoms of an allergic reaction may include rash, itching, swelling, difficulty breathing, or severe dizziness.
- Individuals who experience signs of an allergic reaction should seek medical attention immediately and discontinue the medication until evaluated by a healthcare provider.
Pancreatitis
- Some medications, such as certain DPP-4 inhibitors, have been associated with an increased risk of pancreatitis (inflammation of the pancreas).
- Symptoms of pancreatitis may include severe abdominal pain, nausea, vomiting, and fever. Individuals experiencing these symptoms should seek immediate medical attention.
Bone Fracture Risk
- Long-term use of certain diabetes medications, particularly thiazolidinediones (TZDs), has been associated with an increased risk of bone fractures, particularly in women.
- Healthcare providers may consider bone health assessments and monitoring for individuals at higher risk of fractures.
Kidney Function
- Some diabetes medications, such as SGLT2 inhibitors, may affect kidney function and require monitoring of kidney function parameters.
- Individuals with pre-existing kidney disease or risk factors for kidney problems should be closely monitored while taking these medications.
Cardiovascular Effects
- While many diabetes medications offer cardiovascular benefits, some may have potential cardiovascular risks. For example, certain TZDs have been associated with an increased risk of heart failure.
- Healthcare providers should assess individual cardiovascular risk profiles and consider cardiovascular outcomes when selecting diabetes medications.
Alternatives of Medications To Lower A1C
In addition to medications, several lifestyle modifications and alternative therapies can help lower A1C levels in individuals with diabetes. While these approaches may not replace medications entirely, they can complement conventional treatment and contribute to improved blood sugar control. Here are some alternatives to medications for lowering A1C:
Diet and Nutrition

- Adopting a healthy diet that focuses on whole, unprocessed foods, including fruits, vegetables, whole grains, lean proteins, and healthy fats, can help regulate blood sugar levels.
- Limiting the intake of refined carbohydrates, sugary foods and beverages, and foods high in saturated and trans fats can aid in controlling blood sugar spikes.
- Portion control and mindful eating practices can help prevent overeating and stabilize blood sugar levels throughout the day.
Regular Physical Activity
- Engaging in regular physical activity, such as brisk walking, jogging, cycling, swimming, or strength training, helps improve insulin sensitivity and glucose uptake by muscles.
- Aim for at least 150 minutes of moderate-intensity aerobic activity or 75 minutes of vigorous-intensity aerobic activity per week, spread out over several days.
- Incorporate strength training exercises at least two days per week to build muscle mass and further enhance insulin sensitivity.
Weight Management
- Maintaining a healthy weight or achieving weight loss, if overweight or obese, can significantly improve insulin sensitivity and blood sugar control.
- A combination of dietary changes and regular physical activity is essential for successful weight management.
- Set realistic weight loss goals and track progress over time, making adjustments to diet and exercise as needed.
Blood Sugar Monitoring
- Regular monitoring of blood sugar levels using a home blood glucose meter can provide valuable insights into how different foods, activities, and lifestyle factors affect blood sugar levels throughout the day.
- Use blood sugar data to make informed decisions about dietary choices, exercise routines, and medication adjustments in collaboration with a healthcare provider.
Conclusion
Medications play a significant role in achieving target A1C levels, alongside lifestyle changes such as diet, exercise, and regular monitoring of blood sugar levels.
Understanding the various classes of medications, how they work, their benefits, potential side effects, and other essential considerations empowers individuals and healthcare providers to make informed decisions regarding diabetes management. Always consult with a healthcare professional for personalized advice and treatment recommendations tailored to your specific needs and circumstances.
Do you want to get rid of diabetes? Join our online diabetes treatment program and reverse Diabetes naturally through lifestyle changes such as a Personalized Diet plan, Exercise, Yoga, dieticians, and health coaches.

