Hypoglycemia, often referred to as low blood sugar, is a condition characterized by a decrease in the level of glucose in the blood below normal. It can occur in individuals with diabetes who are taking medications to lower their blood sugar levels. Managing hypoglycemia involves understanding the medications used to treat diabetes and implementing strategies to prevent and treat low blood sugar episodes effectively. This blog covers all the types of Hypoglycemia Medication available, along with its side effects and benefits.
Contents
What is Hypoglycemia?
Hypoglycemia, often referred to as low blood sugar, occurs when the level of glucose (sugar) in the blood drops below normal levels. Glucose is the primary source of energy for the body’s cells, including the brain. Maintaining stable blood sugar levels is essential for overall health and proper functioning of the body.
In individuals without diabetes, the body maintains blood sugar levels within a narrow range through a complex system involving hormones such as insulin and glucagon, which are produced by the pancreas. When blood sugar levels drop, the pancreas releases glucagon, which signals the liver to release stored glucose into the bloodstream, raising blood sugar levels. Conversely, when blood sugar levels rise, the pancreas releases insulin, which helps cells take up glucose from the blood, lowering blood sugar levels.
However, in people with diabetes, this regulatory system may not function properly. In type 1 diabetes, the pancreas produces little to no insulin, while in type 2 diabetes, the body becomes resistant to insulin’s effects or does not produce enough insulin to meet the body’s needs. As a result, blood sugar levels can become too low if too much insulin is taken, not enough food is consumed, or excessive physical activity occurs without adequate carbohydrate intake.
Is Medication Effective for Hypoglycemia?
Medications are not typically used to treat hypoglycemia itself, as hypoglycemia is characterized by low blood sugar levels. Instead, medications are often the cause of hypoglycemia, particularly in individuals with diabetes who are taking medications to lower their blood sugar levels.
The effectiveness of medications in managing hypoglycemia depends on the underlying cause and the specific medication being used. In the context of diabetes management, medications such as insulin and certain oral diabetes medications (e.g., sulfonylureas, and meglitinides) are effective in lowering blood sugar levels and controlling diabetes when used appropriately. However, these medications can sometimes cause hypoglycemia if the dose is too high, if meals are delayed or skipped, or if there is excessive physical activity without adjusting medication doses.
When hypoglycemia occurs as a result of diabetes medications, the primary treatment involves raising blood sugar levels quickly by consuming fast-acting carbohydrates such as glucose tablets, fruit juice, or regular soda. Glucagon injections may be necessary for severe hypoglycemia if the individual is unable to consume oral carbohydrates.
List of Best Hypoglycemia Medication
Determining the “best” hypoglycemia medication depends on various factors such as the individual’s type of diabetes, overall health, other medical conditions, and medication tolerability. Different medications work in different ways to lower blood sugar levels and may have varying risks of causing hypoglycemia. Here’s a list of some commonly prescribed hypoglycemia medications:
Insulin

Insulin therapy is a cornerstone of diabetes management, particularly for individuals with type 1 diabetes and some people with type 2 diabetes who cannot achieve adequate blood sugar control with oral medications alone. Also, Insulin is administered via subcutaneous injections or through an insulin pump, which delivers a continuous infusion of insulin under the skin.
There are several types of insulin, categorized based on their onset, peak action, and duration of action:
- Rapid-acting insulin: These insulins begin to work within 15 minutes after injection, peak within 1-2 hours, and last for 3-4 hours. Examples include insulin lispro (Humalog), insulin aspart (NovoLog), and insulin glulisine (Apidra). They are typically used to cover meals and correct high blood sugar levels.
- Short-acting insulin: Short-acting insulins start working within 30 minutes after injection, peak within 2-3 hours, and last for about 3-6 hours. Regular insulin (Humulin R, Novolin R) is an example of short-acting insulin. It is often used to cover meals or as part of a sliding scale regimen to correct high blood sugar levels.
- Intermediate-acting insulin: These insulins have a slower onset of action and a more prolonged duration compared to rapid-acting and short-acting insulins. They typically start working within 1-2 hours after injection, peak within 4-8 hours, and last for about 12-18 hours. NPH insulin (Humulin N, Novolin N) is an example of intermediate-acting insulin. It is often used as part of basal insulin therapy to provide background insulin coverage throughout the day.
- Long-acting insulin: Long-acting insulins have a slow and consistent onset of action, with no pronounced peak. They provide basal insulin coverage for an extended period, typically lasting 18-24 hours or more. Examples include insulin glargine (Lantus, Basaglar), insulin detemir (Levemir), and insulin degludec (Tresiba).
Sulfonylureas
Sulfonylureas are a class of oral medications commonly used to treat type 2 diabetes. They work by stimulating the pancreas to release more insulin, which helps lower blood sugar levels. While sulfonylureas are effective at reducing blood sugar levels, they are also associated with a higher risk of hypoglycemia compared to some other diabetes medications. Therefore, while sulfonylureas can be effective for certain individuals with type 2 diabetes, they may not always be considered the “best” hypoglycemia medications for everyone.
Here are some key points to consider about sulfonylureas as hypoglycemia medications:
- Effectiveness: Sulfonylureas are effective at lowering blood sugar levels by stimulating insulin secretion from the pancreas. They can help improve glycemic control in people with type 2 diabetes, particularly those who have not achieved target blood sugar levels with lifestyle modifications alone.
Meglitinides
Meglitinides are another class of oral medications used to treat type 2 diabetes. Similar to sulfonylureas, meglitinides work by stimulating the pancreas to release insulin, which helps lower blood sugar levels. While they share a mechanism of action with sulfonylureas, meglitinides have some differences that may make them suitable alternatives for certain individuals, particularly those who are at a higher risk of hypoglycemia.
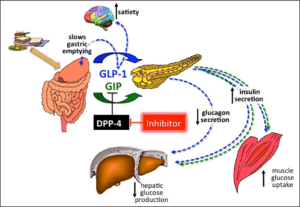
Dipeptidyl Peptidase-4 (DPP-4) Inhibitors
Meglitinides are another class of oral medications used to treat type 2 diabetes. Similar to sulfonylureas, meglitinides work by stimulating the pancreas to release insulin, which helps lower blood sugar levels. While they share a mechanism of action with sulfonylureas, meglitinides have some differences that may make them suitable alternatives for certain individuals, particularly those who are at a higher risk of hypoglycemia.
Here are some key points about meglitinides as hypoglycemia medications:
- Mechanism of Action: Meglitinides, including repaglinide (Prandin) and nateglinide (Starlix), work by binding to ATP-dependent potassium channels on pancreatic beta cells, leading to insulin secretion. They have a rapid onset of action and a shorter duration of action compared to sulfonylureas, making them particularly useful for controlling postprandial (after-meal) blood sugar spikes.
- Reduced Risk of Prolonged Hypoglycemia: One advantage of meglitinides over sulfonylureas is their shorter duration of action, which may reduce the risk of prolonged hypoglycemia if a meal is skipped or delayed. Meglitinides are typically taken before meals to stimulate insulin secretion in response to food intake, and their effects wear off more quickly between meals.
- Lower Risk of Weight Gain: Compared to some other diabetes medications, such as sulfonylureas and insulin, meglitinides are associated with a lower risk of weight gain. This may be beneficial for individuals who are concerned about weight management or who are at risk of obesity-related complications.
- Individual Considerations: While meglitinides can help lower blood sugar levels and reduce the risk of hypoglycemia, they may not be suitable for everyone. Individuals with impaired liver function or those who are prone to frequent episodes of hypoglycemia may need to use meglitinides with caution or under close medical supervision.
Glucagon-like Peptide-1 (GLP-1) Receptor Agonists
Glucagon-like Peptide-1 (GLP-1) receptor agonists are a class of medications used in the management of type 2 diabetes. They mimic the action of the natural hormone GLP-1, which is released by the intestines in response to food intake. GLP-1 receptor agonists work by activating GLP-1 receptors in the pancreas, leading to increased insulin secretion, decreased glucagon secretion, slowed gastric emptying, and increased feelings of satiety.
Here are some key points about GLP-1 receptor agonists as hypoglycemia medications:
- Mechanism of Action: GLP-1 receptor agonists mimic the action of GLP-1, a hormone released by the intestines in response to food intake. By activating GLP-1 receptors in the pancreas, GLP-1 receptor agonists stimulate insulin secretion in a glucose-dependent manner and suppress glucagon secretion, leading to improved blood sugar control.
- Cardiovascular Benefits: Some GLP-1 receptor agonists have been shown to have cardiovascular benefits, including a reduction in the risk of major adverse cardiovascular events (MACE) such as heart attack, stroke, and cardiovascular death. These cardiovascular benefits make GLP-1 receptor agonists attractive options for individuals with type 2 diabetes who are at high risk of cardiovascular disease.
- Once-Weekly Formulations: Several GLP-1 receptor agonists are available in once-weekly formulations, which offer convenience and may improve treatment adherence compared to daily injections. Once-weekly formulations provide sustained blood sugar control over a week, reducing the frequency of injections and potential fluctuations in blood sugar levels.
How To Take Hypoglycemia Medications?

Taking hypoglycemia medications effectively involves several important steps to ensure optimal blood sugar control. Here are some general guidelines for taking hypoglycemia medications:
- Follow Healthcare Provider’s Instructions: Always follow your healthcare provider’s instructions regarding the timing, dosage, and administration of your hypoglycemia medications. Your healthcare provider will prescribe the appropriate medication(s) based on your type of diabetes, overall health, and individual needs.
- Take Medications as Prescribed: Take your hypoglycemia medications exactly as prescribed by your healthcare provider. This includes taking the correct dose at the prescribed times and following any specific instructions provided, such as whether to take the medication with food or on an empty stomach.
- Monitor Blood Sugar Levels: Monitor your blood sugar levels regularly as directed by your healthcare provider. This may involve using a glucometer to measure your blood sugar levels at home or using a continuous glucose monitoring (CGM) system. Regular monitoring helps you track your blood sugar levels and make adjustments to your medication regimen as needed.
- Be Consistent with Meal Timing: Take your hypoglycemia medications according to your meal schedule. Some medications, such as rapid-acting insulin or certain oral medications, may need to be taken with meals to help control postprandial blood sugar levels. Consistent meal timing helps ensure that your medication is properly timed to match your body’s insulin needs.
- Eat Balanced Meals and Snacks: Maintain a balanced diet that includes a variety of nutrient-rich foods, including complex carbohydrates, lean proteins, healthy fats, fruits, and vegetables. Eating balanced meals and snacks throughout the day helps stabilize blood sugar levels and reduces the risk of hypoglycemia.
- Adjust Medications as Needed: Work closely with your healthcare provider to adjust your medication regimen as needed based on changes in your blood sugar levels, diet, physical activity, and overall health.
Conclusion
Hypoglycemia medication plays a vital role in the management of diabetes, but it can sometimes lead to low blood sugar episodes if not used appropriately. By understanding the different classes of hypoglycemia medication and implementing strategies to prevent and manage hypoglycemia effectively, individuals with diabetes can achieve better blood sugar control and improve their overall quality of life. Working closely with healthcare providers and maintaining open communication is key to successful diabetes management and reducing the risk of hypoglycemia.

