Diabetic amyotrophy can present unique challenges, affecting both the physical and emotional well-being of individuals. However, incorporating targeted physical therapy into your routine can significantly enhance mobility, alleviate discomfort, and improve overall quality of life. In this blog, we will explore the intricacies of the condition and delve into effective diabetic amyotrophy physical therapy strategies to manage its symptoms.
Contents
What Is Diabetic Amyotrophy?
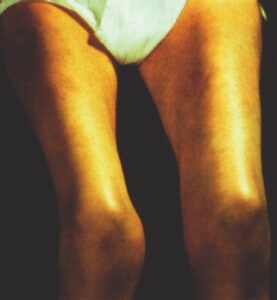 Diabetic amyotrophy is also known as proximal diabetic neuropathy or diabetic lumbosacral radiculoplexus neuropathy. It is a distinct neurological complication associated with diabetes mellitus. This condition primarily affects the lower limbs, causing weakness, pain, and muscle atrophy. Diabetic amyotrophy is characterized by damage to the nerves in the lumbosacral plexus, leading to dysfunction in the muscles of the thighs, hips, and buttocks.
Diabetic amyotrophy is also known as proximal diabetic neuropathy or diabetic lumbosacral radiculoplexus neuropathy. It is a distinct neurological complication associated with diabetes mellitus. This condition primarily affects the lower limbs, causing weakness, pain, and muscle atrophy. Diabetic amyotrophy is characterized by damage to the nerves in the lumbosacral plexus, leading to dysfunction in the muscles of the thighs, hips, and buttocks.
Individuals with diabetes, particularly those with poorly controlled blood sugar levels, are at an increased risk of developing diabetic amyotrophy. The exact mechanisms underlying its development are not fully understood. However, it is believed to involve a combination of vascular, metabolic, and immune factors. Symptoms often manifest gradually, and the condition can significantly impact mobility and daily activities, emphasizing the importance of early recognition and comprehensive management strategies.
What Is The Role Of Physical Therapy In Diabetic Amyotrophy?
The role of physical therapy in diabetic amyotrophy is pivotal in managing the symptoms and enhancing the overall well-being of individuals affected by this condition. Physical therapy aims to address the specific muscle weakness, pain, and functional limitations associated with diabetic amyotrophy through targeted interventions. Therapists work collaboratively with patients to design personalized exercise programs that focus on strengthening weakened muscles, improving flexibility, and enhancing overall mobility.
This therapy plays a crucial role in mitigating the impact of diabetic amyotrophy on daily activities by incorporating a combination of exercises tailored to the individual’s needs. These exercises often include both resistance training and range of motion exercises to address muscle weakness and stiffness. Additionally, therapists may introduce balance and coordination exercises to improve overall stability and reduce the risk of falls, which can be heightened in individuals with diabetic amyotrophy.
The goal is to empower individuals to actively participate in their care, promoting long-term management of symptoms and fostering an improved quality of life. The comprehensive approach of physical therapy addresses the physical aspects of diabetic amyotrophy. And also contributes to the overall well-being of individuals by promoting a proactive and holistic approach to their health.
What Are The Approaches Used In Diabetic Amyotrophy Physical Therapy?
 Diabetic amyotrophy physical therapy employs a multifaceted approach to address the specific challenges associated with this condition. Here are several key approaches used in physical therapy for diabetic amyotrophy:
Diabetic amyotrophy physical therapy employs a multifaceted approach to address the specific challenges associated with this condition. Here are several key approaches used in physical therapy for diabetic amyotrophy:
Strengthening Exercises
Strengthening exercises are a cornerstone of physical therapy for diabetic amyotrophy, targeting the specific muscle groups affected by the condition. Therapists design personalized resistance training programs to address weakness in the thighs, hips, and buttocks. These exercises not only aim to rebuild muscle strength but also contribute to overall functional improvement.
Range of Motion Exercises
Diabetic amyotrophy can lead to stiffness and reduced joint mobility. Range of motion exercises are integral to physical therapy, involving gentle stretching routines to enhance flexibility and maintain joint function. These exercises aim to counteract the limitations imposed by muscle weakness and prevent the development of contractures, contributing to an individual’s ability to move more freely and comfortably.
Balance and Coordination Training
Impaired balance and coordination are common challenges in diabetic amyotrophy. Physical therapists incorporate exercises that focus on improving these aspects, utilizing activities such as standing on one leg, walking on uneven surfaces, and performing controlled movements. By addressing these issues, individuals can reduce their risk of falls and enhance their overall stability, promoting confidence in daily activities.
Low-Impact Activities
Incorporating low-impact activities into the physical therapy regimen is beneficial for cardiovascular health without placing excessive strain on weakened muscles. Activities like swimming, cycling, and walking provide a means to enhance overall fitness and stamina. The low-impact nature of these exercises minimizes stress on joints and muscles, making them suitable for individuals managing diabetic amyotrophy.
Yoga and Tai Chi
Mindful movement practices such as yoga and tai chi offer unique benefits in the context of diabetic amyotrophy. These activities involve slow, controlled movements, promoting flexibility, balance, and relaxation. Yoga, with its emphasis on poses and stretches, and tai chi, with its flowing sequences, contribute to improved body awareness and a strengthened mind-body connection.
Assistive Devices and Adaptive Strategies
Physical therapists play a crucial role in assessing an individual’s mobility and recommending appropriate assistive devices and adaptive strategies. For those with diabetic amyotrophy, mobility aids such as canes or walkers may be suggested to enhance stability and prevent falls. Additionally, therapists guide adaptive strategies for daily living, helping individuals optimize their independence by modifying tasks and environments to accommodate their specific needs.
Pain Management Techniques
 Chronic pain is a common symptom of diabetic amyotrophy, and physical therapists integrate various pain management techniques into their treatment plans. Modalities like heat or cold therapy may be employed to alleviate discomfort and reduce inflammation. Therapists also educate individuals on proper body mechanics and ergonomics to minimize strain on affected muscles. By addressing pain through these approaches, physical therapy not only enhances physical well-being but also contributes to an improved overall quality of life.
Chronic pain is a common symptom of diabetic amyotrophy, and physical therapists integrate various pain management techniques into their treatment plans. Modalities like heat or cold therapy may be employed to alleviate discomfort and reduce inflammation. Therapists also educate individuals on proper body mechanics and ergonomics to minimize strain on affected muscles. By addressing pain through these approaches, physical therapy not only enhances physical well-being but also contributes to an improved overall quality of life.
Education on Lifestyle Modifications
Physical therapists play a crucial role in educating individuals about lifestyle modifications that can positively impact diabetic amyotrophy. This includes guiding on maintaining optimal blood sugar levels through dietary choices and medication adherence. Lifestyle changes, such as adopting a balanced diet and engaging in regular exercise, contribute to better overall health and can have a positive impact on managing the condition.
Monitoring and Adjusting Treatment Plans
A dynamic and responsive approach to physical therapy is essential in managing diabetic amyotrophy. Physical therapists regularly monitor the progress of individuals and adjust treatment plans accordingly. This ongoing assessment allows for modifications to the intensity, duration, and specific exercises to meet evolving needs and challenges. By tailoring the treatment plan to individual responses and goals, physical therapists ensure that therapy remains effective in addressing the dynamic nature of diabetic amyotrophy.
By combining these approaches, diabetic amyotrophy physical therapy aims to enhance muscle strength, improve mobility, and empower individuals to manage their condition effectively. Ultimately promoting a better quality of life.
Is Diabetic Amyotrophy Physical Therapy Painful?
Diabetic amyotrophy physical therapy should not cause significant pain. The goal of physical therapy for conditions like diabetic amyotrophy is to manage symptoms, improve mobility, and enhance overall well-being. Physical therapists design exercise programs that are tailored to an individual’s specific needs, taking into account their pain threshold and the extent of their muscle weakness.
While some exercises might initially cause mild discomfort or fatigue as weakened muscles are engaged, it’s essential to communicate openly with your physical therapist. They can adjust the intensity, duration, or type of exercises based on your feedback to ensure that the sessions are challenging yet manageable.
If you experience pain during or after physical therapy, it’s crucial to inform your therapist promptly. Pain is not the goal of physical therapy, and modifications can be made to the treatment plan to better suit your comfort level. It’s also important to note that some discomfort may arise due to the nature of diabetic amyotrophy itself. Communicating with your healthcare team, including your physical therapist, about any changes in symptoms or pain levels is essential for managing the condition effectively.
What Are Some Limitations To Consider?
 When undergoing physical therapy for diabetic amyotrophy, several limitations and considerations should be kept in mind:
When undergoing physical therapy for diabetic amyotrophy, several limitations and considerations should be kept in mind:
- Individual Variability
The response to physical therapy can vary from person to person. Factors such as the severity of diabetic amyotrophy, overall health, and adherence to the prescribed exercises can influence outcomes.
- Pain Sensitivity
Individuals with diabetic amyotrophy may experience varying levels of pain sensitivity. Physical therapy should be tailored to accommodate individual pain thresholds, and communication with the therapist is crucial to ensure exercises are challenging but not excessively painful.
- Progression Rate
Improvement in symptoms and function may occur at a gradual pace. Patience is essential, and expectations should be realistic. Consistent effort and adherence to the physical therapy plan are crucial for long-term success.
- Coexisting Medical Conditions
Individuals with diabetic amyotrophy often have other medical conditions related to diabetes or general health. These conditions may impact the ability to engage in certain types of exercises or influence the overall rehabilitation process.
- Motivation and Adherence
The success of physical therapy relies on the individual’s motivation and commitment to the prescribed exercises and lifestyle modifications. Adherence to the treatment plan is crucial for achieving positive outcomes.
- Cognitive Function
Some individuals with diabetic amyotrophy may also experience cognitive impairments or complications related to diabetes. This may affect the ability to understand and follow the physical therapy instructions.
- Potential for Fluctuating Symptoms
Symptoms of diabetic amyotrophy may fluctuate over time. Periods of improvement or exacerbation may occur, necessitating adjustments to the physical therapy plan and overall management approach.
Overall, regular reassessment of goals, modifications to the treatment plan, and addressing any emerging concerns or limitations contribute to a more effective and personalized rehabilitation experience.
Conclusion
In conclusion, navigating life with diabetic amyotrophy is undoubtedly challenging, but by embracing a holistic approach that includes physical therapy, individuals can take significant steps towards managing symptoms and improving overall well-being. Through targeted exercises, balance training, and adaptive strategies, physical therapy empowers individuals to regain strength, flexibility, and confidence in their daily lives.
The journey of diabetic amyotrophy physical therapy involves patience and persistence, with the understanding that progress may be gradual. Beyond the physical aspect, addressing emotional well-being, incorporating healthy lifestyle modifications, and seeking support form integral parts of the comprehensive care plan. Do you want to get rid of diabetes? Join our online diabetes treatment program and reverse Diabetes naturally through lifestyle changes such as a Personalized Diet plan, Exercise, Yoga, dieticians, and health coaches.

