Diabetic leg ulcers are a common and serious complication that can arise from diabetes. These ulcers are chronic wounds that develop on the lower extremities, particularly the feet and are often challenging to manage. Effective diabetic leg ulcer treatment involves a multidisciplinary approach, combining medical intervention, wound care, and lifestyle modifications. In this comprehensive guide, we will explore the causes, symptoms, and various treatment options for diabetic leg ulcers, as well as strategies for prevention.
Contents
- 1 What are Diabetes Leg Ulcers?
- 2 List of Diabetes Leg Ulcers Treatment Methods
- 2.1 Wound Care
- 2.2 Infection Management
- 2.3 Blood Sugar Control:
- 2.4 Vascular Interventions
- 2.5 Advanced Therapies
- 2.6 Compression Therapy
- 2.7 Pain Management
- 2.8 Nutritional Support
- 2.9 Physical Therapy
- 2.10 Psychosocial Support
- 2.11 Bioengineered Skin Substitutes:
- 2.12 Electrical Stimulation
- 2.13 Infrared Light Therapy
- 2.14 Negative Pressure Wound Therapy (NPWT)
- 2.15 Limb Elevation
- 3 Conclusion
What are Diabetes Leg Ulcers?

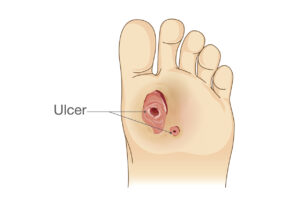
Diabetic leg ulcers result from a combination of factors, primarily stemming from poor blood circulation and nerve damage associated with diabetes. Elevated blood sugar levels can lead to peripheral artery disease (PAD) and peripheral neuropathy, reducing blood flow and sensation in the lower limbs. Consequently, minor injuries or cuts may go unnoticed, allowing them to develop into ulcers.
Symptoms of Diabetic Leg Ulcers:
- Persistent redness or discoloration
- Swelling in the affected area
- Open sores or wounds that are slow to heal
- Presence of pus or discharge
- Foul odor from the wound
- Pain or tenderness
- Warmth or heat in the affected region
List of Diabetes Leg Ulcers Treatment Methods
Diabetic leg ulcers are a serious complication that requires a comprehensive and multidisciplinary approach for effective treatment. Here, we will delve into various treatment methods specifically targeted at managing diabetic leg ulcers.
Wound Care
Wound care is a fundamental aspect of diabetic leg ulcer treatment, aiming to create an optimal environment for healing and prevent infection.
Cleaning and Dressing: Cleaning the ulcer and changing dressings regularly is vital to remove debris, bacteria, and dead tissue. Physicians may recommend the use of antiseptic solutions or sterile saline to cleanse the wound. Specialized dressings, such as hydrocolloids or foams, are employed to maintain a moist environment, promote granulation tissue formation, and accelerate the healing process.
Debridement: Debridement involves the removal of dead or infected tissue from the ulcer site. This can be achieved through different methods, including surgical, enzymatic, and autolytic debridement. Surgical debridement is a more invasive procedure performed by healthcare professionals, while enzymatic and autolytic debridement rely on topical agents or the body’s natural processes to break down and remove necrotic tissue.
Infection Management
Addressing infections promptly is crucial in diabetic leg ulcer treatment to prevent complications and promote healing.
Antibiotics: In cases where bacterial infection is present, physicians may prescribe oral or topical antibiotics. These medications help combat bacterial growth, reducing the risk of systemic infection. The choice of antibiotics depends on the type and severity of the infection.
Offloading: Offloading is a strategy to reduce pressure on the affected area, facilitating the healing process. Customized shoes, braces, or crutches may be recommended to redistribute weight and alleviate stress on the ulcer. Offloading is essential for preventing further trauma to the wound and promoting optimal healing conditions.
Blood Sugar Control:
Maintaining optimal blood sugar levels is a foundational aspect of diabetic leg ulcer treatment, as elevated glucose levels impede the healing process.
Optimal Glycemic Control: Achieving tight control of blood sugar levels involves a combination of lifestyle modifications, medication adherence, and regular monitoring. Patients must adhere to dietary restrictions, engage in regular physical activity, and take prescribed medications as directed. Tight glycemic control not only promotes wound healing but also reduces the risk of further complications associated with diabetes.
Vascular Interventions
Peripheral artery disease (PAD) is a common contributor to diabetic leg ulcers, and vascular interventions may be necessary to improve blood flow.
Angioplasty: Angioplasty is a minimally invasive procedure that involves the insertion of a balloon catheter to open narrowed or blocked arteries. This technique can enhance blood flow to the affected limb, promoting tissue oxygenation and supporting the healing of ulcers. Stents may also be placed to maintain vessel patency.
Vascular Surgery: Severe cases of PAD may require surgical intervention. Vascular surgery aims to address arterial blockages, bypass damaged vessels, or create new pathways for blood circulation. Revascularization procedures can be instrumental in restoring adequate blood supply to the affected extremity.
Advanced Therapies
In cases where conventional treatments may be insufficient, advanced therapies can provide additional support for diabetic leg ulcer healing.
Hyperbaric Oxygen Therapy: Hyperbaric oxygen therapy involves breathing pure oxygen in a pressurized room or chamber. This increases the amount of oxygen in the bloodstream, promoting tissue repair and regeneration. Hyperbaric oxygen therapy can be particularly beneficial in cases where wounds are slow to heal due to compromised oxygen delivery.
Cellular and Tissue-Based Products: Advanced wound care products, such as growth factors, stem cells, and tissue grafts, are used to stimulate tissue regeneration. These products can enhance the natural healing process and accelerate the closure of diabetic leg ulcers. Cellular and tissue-based therapies are continually evolving, offering promising avenues for improving treatment outcomes.
Compression Therapy
Compression therapy is a widely used approach to manage edema and improve blood circulation in the lower extremities.
Applying compression bandages or stockings helps reduce swelling and venous congestion in the affected limb. This external pressure aids in preventing the accumulation of fluids, supporting venous return, and promoting overall vascular health. Properly fitted compression garments are essential to avoid complications such as skin irritation or compromised arterial circulation.
Pain Management
Managing pain associated with diabetic leg ulcers is crucial for improving the patient’s quality of life and promoting adherence to the treatment plan.
Prescription or over-the-counter analgesics may be recommended to alleviate pain. Additionally, healthcare providers may suggest the use of topical agents containing lidocaine or other pain-relieving components to provide localized relief.
Nutritional Support
Nutritional support plays a vital role in the healing process, as adequate nutrients are essential for tissue repair and regeneration.
Patients with diabetic leg ulcers should follow a well-balanced diet rich in protein, vitamins, and minerals. Protein is particularly important for collagen synthesis, a key component in wound healing. Nutritional supplements may be prescribed if dietary intake is insufficient to meet the body’s demands for healing.
Physical Therapy
Physical therapy can be beneficial in improving mobility, preventing muscle atrophy, and addressing gait abnormalities associated with diabetic leg ulcers.
Customized exercise programs and stretching routines can enhance circulation, improve muscle strength, and promote overall joint health. Physical therapists work with patients to develop tailored plans that accommodate their specific needs and capabilities.
Psychosocial support is integral to diabetic leg ulcer treatment, addressing the emotional and mental well-being of patients.
Counseling and Support Groups: Living with chronic wounds can be emotionally challenging. Counseling and participation in support groups provide patients with an outlet to express their concerns, share experiences, and receive guidance on coping strategies. Mental well-being is interconnected with physical health, and addressing both aspects contributes to a more comprehensive healing process.
Bioengineered Skin Substitutes:
Bioengineered skin substitutes represent a cutting-edge approach to diabetic leg ulcer treatment, leveraging advanced materials and technologies.
Application of Skin Grafts: Bioengineered skin grafts offer several advantages. These grafts can be tailored to match the patient’s specific needs, promoting improved adherence and compatibility. Additionally, they often provide a more effective barrier against infection and can accelerate the formation of new tissue. The choice between autografts, allografts, and xenografts depends on factors such as the size and depth of the ulcer, as well as the patient’s overall health.
Cultured Epidermal Autografts: In cases where a patient’s skin is not sufficient for grafting, cultured epidermal autografts can be produced in a laboratory setting. This technique involves taking a small skin biopsy, isolating and expanding the epidermal cells, and then grafting the cultured cells back onto the wound. This approach can be particularly useful for extensive or challenging-to-treat ulcers.
Electrical Stimulation
Electrical stimulation has gained attention for its potential to modulate cellular processes and enhance the healing of diabetic leg ulcers.
Electrotherapy Devices: Electrotherapy devices, including electrical stimulation units, deliver controlled electrical currents to the ulcer site. This stimulation is thought to increase cellular activity, promote angiogenesis (formation of new blood vessels), and accelerate the production of growth factors. While research on the efficacy of electrical stimulation is ongoing, some studies suggest its positive impact on wound closure and overall healing outcomes.
Frequency-Specific Microcurrent: Frequency-specific microcurrent (FSM) is a subset of electrical stimulation that utilizes specific frequencies to target different aspects of wound healing. FSM has shown promise in enhancing cellular communication, reducing inflammation, and promoting tissue repair. Research in this area continues to explore optimal frequency parameters for diabetic wound care.
Infrared Light Therapy

Infrared light therapy harnesses the therapeutic potential of specific wavelengths of light to address various aspects of diabetic leg ulcer healing.
Low-Level Laser Therapy (LLLT): LLLT, also known as photobiomodulation, involves the application of low-level lasers or light-emitting diodes (LEDs) to the ulcerated area. This non-thermal light promotes cellular energy production, stimulates mitochondrial function, and enhances tissue repair. LLLT has demonstrated effectiveness in reducing inflammation, and pain, and promoting wound closure.
Near-Infrared (NIR) Light Therapy: NIR light therapy focuses on the use of near-infrared wavelengths, which can penetrate deeper into tissues. This form of light therapy has shown potential in improving blood flow, oxygenation, and collagen production. NIR therapy may contribute to the overall management of diabetic leg ulcers by addressing underlying vascular and tissue health.
Negative Pressure Wound Therapy (NPWT)
Negative Pressure Wound Therapy is a dynamic approach that utilizes controlled negative pressure to create a conducive environment for wound healing.
Vacuum-Assisted Closure (VAC): VAC involves applying a sealed dressing over the wound connected to a vacuum source. Negative pressure helps remove excess fluids, reduce bacterial load, and stimulate the formation of granulation tissue. This technique is particularly beneficial for chronic or non-healing ulcers, offering a unique mechanism to enhance tissue regeneration.
Instillation Therapy: In some cases, NPWT can be combined with instillation therapy, where therapeutic solutions (e.g., saline, antiseptics, or enzymatic solutions) are intermittently introduced into the wound bed. This enhances the removal of infectious material and promotes a more favorable environment for healing.
Limb Elevation
Limb elevation is a straightforward yet effective strategy to complement other interventions in the management of diabetic leg ulcers.
Leg Elevation Techniques: Encouraging patients to elevate their legs above heart level at regular intervals can assist in reducing edema and improving venous return. Elevation can be combined with other therapies to optimize outcomes. It is particularly beneficial for individuals with compromised venous circulation.
Intermittent Pneumatic Compression (IPC): Intermittent pneumatic compression involves the use of inflatable cuffs or sleeves on the legs that intermittently compress and release. This dynamic compression aids in reducing swelling, enhancing blood flow, and preventing blood stasis. IPC can be an effective adjunct to limb elevation in the overall management of diabetic leg ulcers.
Conclusion
Diabetic leg ulcers pose a significant health risk and require a comprehensive approach to treatment. Successful management involves addressing the underlying causes, meticulous wound care, infection control, and lifestyle modifications. Individuals with diabetes should prioritize preventive measures to reduce the risk of developing leg ulcers and work closely with healthcare professionals for timely intervention. By adopting a proactive approach, individuals can enhance their quality of life and reduce the impact of diabetic complications on their overall well-being.
Do you want to get rid of diabetes? Join our online diabetes treatment program and reverse Diabetes naturally through lifestyle changes such as a Personalized Diet plan, Exercise, Yoga, dieticians, and health coaches.

