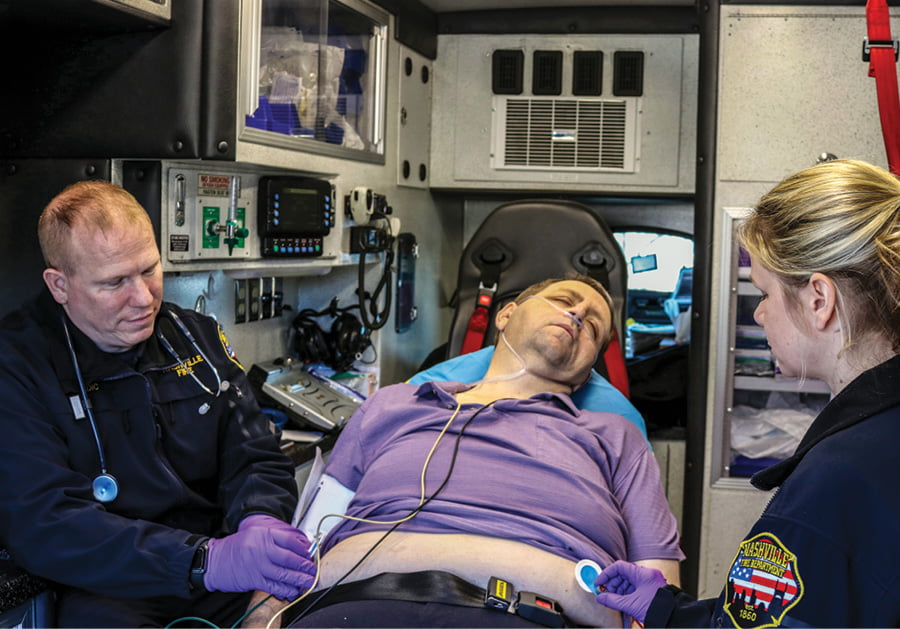
” Coma” is, a severe complication of diabetes, is a life-threatening condition that requires immediate medical attention. It occurs when blood sugar levels become dangerously high (hyperglycemia) or dangerously low (hypoglycemia), leading to a state of unconsciousness. This blog aims to provide a detailed overview of diabetic coma, its causes, symptoms, and, most importantly, the various treatment options available to manage this critical condition.
Contents
What is a Diabetic Coma?

A diabetic coma is a serious and life-threatening complication of diabetes that occurs when there is a significant imbalance in blood sugar levels. It is characterized by either extremely high blood sugar (hyperglycemia) or dangerously low blood sugar (hypoglycemia), leading to a state of unconsciousness. This condition is a medical emergency that requires immediate attention and intervention.
There are two main types of diabetic coma:
Hyperglycemic Diabetic Coma:
- Cause: This type of coma is primarily associated with very high blood sugar levels, often resulting from uncontrolled diabetes.
- Mechanism: When there is insufficient insulin or the body is unable to use insulin effectively, glucose cannot enter cells to provide energy. As a result, blood sugar levels rise dramatically.
- Symptoms: Extreme thirst, frequent urination, fatigue, confusion, nausea, and vomiting.
- Triggers: Uncontrolled diabetes, illness, infection, or inadequate insulin administration.
Hypoglycemic Diabetic Coma:
- Cause: This type of coma is linked to severely low blood sugar levels, usually due to an excess of insulin or insufficient carbohydrate intake.
- Mechanism: Too much insulin or not enough glucose in the bloodstream prevents the brain from receiving the energy it needs, leading to unconsciousness.
- Symptoms: Sweating, trembling, rapid heartbeat, dizziness, weakness, confusion, and irritability.
- Triggers: Insulin overdose, skipping meals, intense physical activity without adequate carbohydrate intake.
Different Diabetic Coma Treatment Methods
The treatment of diabetic coma depends on whether it is caused by hyperglycemia (high blood sugar) or hypoglycemia (low blood sugar). Both situations are medical emergencies requiring immediate attention. Here are the different treatment methods for each type of diabetic coma:
Hyperglycemic Diabetic Coma Treatment
- Insulin Therapy: Hyperglycemic diabetic coma is a result of elevated blood sugar levels, often due to insufficient insulin or insulin resistance. Intravenous administration of regular insulin is crucial for lowering blood glucose rapidly. Continuous monitoring allows healthcare professionals to adjust the insulin dosage to bring blood sugar levels back to a safe range. In some cases, subcutaneous insulin may be used once the person is stabilized. The overall goal is to enhance glucose utilization, reduce circulating glucose levels, and address the metabolic imbalances associated with hyperglycemia.
- Fluid Replacement: Hyperglycemic coma is frequently accompanied by dehydration due to excessive urination and fluid loss. Intravenous fluid replacement is essential to correct dehydration and restore electrolyte balance. Fluids also help improve blood circulation and organ function. The choice of fluids may include normal saline or balanced electrolyte solutions. Careful monitoring of fluid intake is crucial to prevent complications such as fluid overload. Fluid replacement is an integral part of hyperglycemic diabetic coma treatment, complementing insulin therapy to address both the immediate and underlying causes of the condition.
- Electrolyte Replacement: Hyperglycemia can lead to imbalances in electrolytes such as potassium, sodium, and chloride. Intravenous electrolyte replacement may be necessary to restore proper balance and prevent complications like cardiac arrhythmias. Regular monitoring of electrolyte levels guides healthcare professionals in adjusting the electrolyte replacement regimen as needed. Electrolyte replacement complements fluid therapy and contributes to the comprehensive management of hyperglycemic diabetic coma.
- Identifying and Treating Underlying Causes: Addressing the root causes of hyperglycemia is crucial for effective treatment. If an infection is present, antibiotics may be prescribed. Healthcare professionals investigate and manage any underlying illnesses or medication issues contributing to the hyperglycemic state. A thorough assessment guides targeted interventions to prevent the recurrence of hyperglycemic episodes.
Hypoglycemic Diabetic Coma Treatment
- Glucose Administration: Hypoglycemic diabetic coma results from critically low blood sugar levels, often due to an excess of insulin or inadequate carbohydrate intake. Rapid administration of glucose is the cornerstone of treatment. Intravenous glucose is administered to provide an immediate and concentrated source of energy. Dextrose solutions are commonly used for intravenous glucose administration.
- Continuous Monitoring: After the initial glucose administration, continuous monitoring of blood glucose levels is imperative. Frequent blood glucose checks help healthcare providers assess the response to treatment and make necessary adjustments. Continuous monitoring is essential for preventing a recurrence of hypoglycemia and maintaining stable blood sugar levels. For individuals with diabetes, continuous monitoring is an integral part of self-care, enabling them to identify trends, understand the impact of various factors on blood sugar levels, and make informed decisions about their daily management.
- Identifying and Addressing Triggers: The identification and management of specific triggers contributing to hypoglycemia are vital for long-term care. This involves a comprehensive review of the individual’s medication regimen, meal plans, and lifestyle factors. Adjustments may be made to insulin dosages, meal timings, or types of insulin used. Patient education is crucial in empowering individuals to recognize and address potential triggers on their own. It also helps in fostering proactive management and prevention strategies.
- Intramuscular Glucagon: In severe cases where the person is unconscious or unable to swallow, intramuscular glucagon may be administered. Glucagon is a hormone that stimulates the release of glucose from the liver, raising blood sugar levels. Family members or caregivers are often trained to administer intramuscular glucagon in emergencies. However, it’s important to note that this is typically a secondary intervention, and the primary goal is to restore blood sugar levels through intravenous glucose administration when possible.
How To Get Diabetic Coma Treatment?