Diabetes mellitus, often referred to simply as diabetes, is a chronic medical condition that affects millions of people worldwide. Characterized by elevated blood sugar levels, diabetes can lead to various complications, including cardiovascular disease, kidney failure, and nerve damage. While diabetes management has improved significantly over the years, there is an ongoing quest for a definitive cure. In this blog, we will delve into the complexities of diabetes mellitus, explore current research efforts, and examine potential avenues for a cure.
Contents
- 1 Understanding Diabetes Mellitus
- 2 Is It Easy To Cure Diabetes Mellitus?
- 3 Various Diabetes Mellitus Cure Methods
- 3.1 Beta Cell Regeneration
- 3.2 Immunotherapy
- 3.3 Genetic Approaches
- 3.4 Artificial Pancreas
- 3.5 Metabolic Surgery
- 3.6 Stem Cell Therapy
- 3.7 Vaccine Research
- 3.8 Islet Cell Transplantation
- 3.9 GLP-1 Receptor Agonists
- 3.10 SGLT-2 Inhibitors
- 3.11 Gut Microbiota Modulation
- 3.12 Anti-Inflammatory Therapies
- 3.13 Exercise and Physical Activity
- 3.14 Dietary Interventions
- 3.15 Nanotechnology and Drug Delivery Systems
- 4 Challenges and Considerations in Diabetes Mellitus Cure
- 5 Conclusion
Understanding Diabetes Mellitus
Diabetes mellitus is a chronic metabolic disorder characterized by elevated levels of glucose in the blood. This condition results from the body’s inability to produce enough insulin or effectively use the insulin it produces. Insulin is a hormone crucial for regulating blood sugar (glucose) levels and facilitating the uptake of glucose by cells for energy.
1. Type 1 Diabetes:
- Cause: Autoimmune response leading to the destruction of insulin-producing beta cells in the pancreas.
- Onset: Usually occurs in childhood or adolescence.
- Treatment: Requires lifelong insulin injections or an insulin pump.
2. Type 2 Diabetes:
- Cause: Insulin resistance, where cells do not respond properly to insulin, and decreased insulin production over time.
- Onset: Typically develops in adulthood, but can occur at any age.
- Treatment: Managed through lifestyle changes, oral medications, injectable medications, and, in some cases, insulin.
3. Gestational Diabetes:
- Occurrence: Develops during pregnancy.
- Risk: Increases the risk of type 2 diabetes for both the mother and child.
- Management: Diet, exercise, and, in some cases, insulin.
Is It Easy To Cure Diabetes Mellitus?
there is no easy or immediate cure for diabetes mellitus. Diabetes is a complex and chronic medical condition that requires lifelong management rather than a quick fix. It is essential to differentiate between managing diabetes effectively and finding a complete cure.
Several factors contribute to the complexity of diabetes:
- Heterogeneity: Diabetes is not a one-size-fits-all condition. There are different types, including Type 1, Type 2, and gestational diabetes, each with its causes, risk factors, and management strategies.
- Multifactorial Causes: The development of diabetes involves a combination of genetic, environmental, and lifestyle factors. Addressing these factors comprehensively is challenging.
- Chronic Nature: Diabetes is a chronic condition that often requires long-term management to control blood glucose levels and prevent complications.
- Autoimmune Involvement (Type 1): Type 1 diabetes involves an autoimmune response where the body’s immune system attacks and destroys insulin-producing beta cells in the pancreas. Reversing this autoimmune process is a significant challenge.
- Insulin Resistance (Type 2): In Type 2 diabetes, insulin resistance and reduced insulin production are common issues. Lifestyle changes, medication, and sometimes insulin therapy are needed to manage the condition effectively.
Various Diabetes Mellitus Cure Methods
Ongoing research has explored various approaches to managing the condition more effectively and potentially finding a cure. Here are several methods and avenues being investigated:
Beta Cell Regeneration
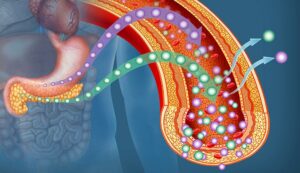
Beta cells, responsible for producing insulin in the pancreas, are crucial for glucose regulation.
- In Type 1 diabetes, these cells are attacked by the immune system, while in Type 2 diabetes, their functionality diminishes over time.
- The approach of beta cell regeneration involves exploring ways to restore or replace these cells.
- Researchers are investigating the use of stem cells and other cellular therapies to regenerate beta cells and reinstate normal insulin production.
The aim is to develop treatments that can effectively replenish the body’s insulin-producing capacity.
Immunotherapy
Type 1 diabetes is characterized by an autoimmune response that destroys insulin-producing beta cells. Immunotherapy seeks to modulate the immune response to prevent the ongoing destruction of these cells.
This may involve interventions to suppress the autoimmune response selectively without compromising the overall function of the immune system.
Immunotherapeutic approaches are being explored to preserve and protect beta cell function, offering a potential way to halt or slow the progression of Type 1 diabetes.
Genetic Approaches
Understanding the genetic factors contributing to diabetes is fundamental for developing targeted interventions. Gene editing technologies, such as CRISPR-Cas9, are being investigated to correct genetic mutations associated with diabetes.
The goal is to tailor treatments based on an individual’s genetic profile, addressing the specific genetic factors contributing to their diabetes. Precision medicine approaches may play a significant role in the future of diabetes care, offering personalized treatments based on a person’s unique genetic makeup.
Artificial Pancreas
Advancements in technology have led to the development of artificial pancreas systems. These systems integrate continuous glucose monitoring with automated insulin delivery.
- By mimicking the function of a healthy pancreas, these devices automatically adjust insulin delivery in response to real-time glucose levels.
- While not a cure, artificial pancreas systems significantly improve blood sugar control and reduce the burden on individuals with diabetes, enhancing their quality of life.
Metabolic Surgery
Originally designed for weight loss, certain types of bariatric surgery have shown positive effects on glucose metabolism.
- Metabolic surgery, such as gastric bypass, leads to rapid improvements in insulin sensitivity and can induce diabetes remission in some cases.
- The mechanisms behind these metabolic effects are still being studied, but the approach holds promise as an unconventional method for managing and potentially reversing diabetes.
Stem Cell Therapy

Stem cells, with their ability to differentiate into various cell types, are being explored for their potential to generate insulin-producing cells. Also, Stem cell therapy involves using these cells, either derived from the patient’s own body or from other sources, to generate functional beta cells.
The goal is to transplant these cells into the pancreas, restoring the body’s ability to produce insulin. While still in the experimental stage, stem cell therapy represents an exciting avenue for potential diabetes treatment.
Vaccine Research
Researchers are exploring the development of vaccines to modulate the immune response involved in the destruction of beta cells in Type 1 diabetes.
- These vaccines aim to prevent or slow down the progression of the autoimmune response, ultimately preserving beta cell function.
- Vaccine research is in the early stages, and the goal is to develop targeted interventions that can modify the immune system’s behavior specifically related to the autoimmune attack on insulin-producing cells.
Islet Cell Transplantation
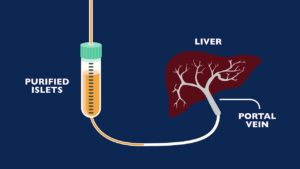
Islet cell transplantation involves transplanting cells containing insulin-producing beta cells into the pancreas. This procedure has shown effectiveness in improving insulin production in individuals with Type 1 diabetes.
Challenges include a shortage of donor cells and the need for immunosuppression to prevent rejection. While providing a potential cure, broader accessibility and refining the transplantation process are areas of ongoing research to make islet cell transplantation a more widely applicable solution.
GLP-1 Receptor Agonists
Glucagon-like peptide-1 (GLP-1) receptor agonists are a class of medications used to treat Type 2 diabetes. They mimic the effects of GLP-1, a hormone that stimulates insulin secretion and reduces glucagon production.
Ongoing research explores the potential of GLP-1 receptor agonists not only for managing diabetes but also for promoting beta cell health and function. Some studies suggest that these medications may have protective effects on beta cells, potentially contributing to disease modification.
SGLT-2 Inhibitors
Sodium-glucose cotransporter-2 (SGLT-2) inhibitors are another class of medications used in Type 2 diabetes treatment. They work by inhibiting glucose reabsorption in the kidneys, leading to increased glucose excretion in the urine.
Some research suggests that SGLT-2 inhibitors may have additional benefits beyond glycemic control. Studies explore their potential in reducing cardiovascular risks and preserving beta cell function, possibly impacting the course of diabetes progression.
Gut Microbiota Modulation
The gut microbiota plays a role in various aspects of health, including metabolism and immune function.
Research is ongoing to understand the relationship between gut microbiota and diabetes. Modulating the gut microbiota through dietary interventions, probiotics, or fecal microbiota transplantation may have potential implications for diabetes management and prevention.
Anti-Inflammatory Therapies
Chronic inflammation is implicated in the development and progression of diabetes.
Therapies targeting inflammation, such as anti-inflammatory drugs or dietary interventions rich in anti-inflammatory compounds, are being explored. Reducing systemic inflammation may contribute to improved insulin sensitivity and better overall metabolic health.
Exercise and Physical Activity

Regular physical activity is known to have numerous health benefits, including improved insulin sensitivity.
Exercise is considered a cornerstone in the management of diabetes. Ongoing research investigates the impact of different exercise regimens on glucose metabolism, insulin sensitivity, and beta cell function. Tailored exercise prescriptions may become part of individualized diabetes management plans.
Dietary Interventions
Diet plays a crucial role in diabetes management, influencing blood sugar levels and overall metabolic health.
Various dietary approaches, including low-carbohydrate diets, Mediterranean diets, and intermittent fasting, are being studied for their impact on glycemic control and diabetes progression. Personalized nutrition plans may become integral to diabetes care.
Nanotechnology and Drug Delivery Systems
Advancements in nanotechnology offer innovative approaches to drug delivery.
Nanoparticles and nanocarriers are being explored for targeted drug delivery to specific cells or tissues, potentially enhancing the efficacy of diabetes medications. This approach aims to improve treatment outcomes while minimizing side effects.
Challenges and Considerations in Diabetes Mellitus Cure

Finding a cure for diabetes mellitus is a complex and challenging endeavor, marked by various hurdles and considerations that researchers and healthcare professionals must navigate. Here are some common challenges and considerations in the quest for a diabetes cure:
1. Heterogeneity of Diabetes:
- Challenge: Diabetes is not a one-size-fits-all condition; it exists in different forms, each with its characteristics and causes.
- Consideration: Developing a cure that addresses the diverse aspects of diabetes requires tailored approaches for different types and stages of the condition.
2. Multifactorial Causes:
- Challenge: Diabetes results from a combination of genetic, environmental, and lifestyle factors.
- Consideration: A successful cure needs to account for this multifactorial nature, addressing both the root causes and the complex interplay of contributing factors.
3. Chronic Nature:
- Challenge: Diabetes is a chronic condition requiring lifelong management.
- Consideration: A cure should not only address the immediate symptoms but also provide a lasting solution, ensuring sustained control over blood sugar levels.
4. Autoimmune Involvement (Type 1):
- Challenge: Type 1 diabetes involves the immune system mistakenly attacking insulin-producing cells.
- Consideration: Any cure for Type 1 diabetes must find a way to halt or reverse the autoimmune process without compromising the overall function of the immune system.
5. Insulin Resistance (Type 2):
- Challenge: Type 2 diabetes often involves insulin resistance and reduced insulin production.
- Consideration: A cure for Type 2 diabetes should focus on restoring insulin sensitivity and addressing the factors contributing to insulin resistance.
6. Long-term Safety and Efficacy:
- Challenge: Developing a cure requires ensuring its safety and long-term effectiveness.
- Consideration: Rigorous testing and monitoring are essential to confirm that a potential cure not only works in the short term but also remains safe and effective over an individual’s lifetime.
Conclusion
The pursuit of a cure for diabetes mellitus is a multifaceted journey that involves understanding the complex interplay of genetic, immunologic, and metabolic factors. While current management strategies provide effective control, the scientific community’s relentless efforts offer hope for a future where diabetes can be cured. As research progresses, collaboration between clinicians, scientists, and individuals living with diabetes will play a pivotal role in bringing about a new era in diabetes care—one where the emphasis shifts from management to eradication.
Do you want to get rid of diabetes? Join our online diabetes treatment program and reverse Diabetes naturally through lifestyle changes such as a Personalized Diet plan, Exercise, Yoga, dieticians, and health coaches.

