For individuals living with diabetes, managing blood sugar levels is a critical aspect of maintaining overall health and well-being. Traditionally, insulin injections have been a cornerstone in the management of diabetes, particularly for those with Type 1 diabetes. However, the daily routine of injections can be challenging for many, leading to a growing interest in alternative methods of insulin delivery and diabetes management. This guide delves into the innovative alternatives to insulin injections, offering new hope and possibilities for those seeking more convenient and less invasive options.
Contents
When To Consider Alternatives To Insulin Injections?
 Considering an alternative to insulin injections is a decision that should be made in close consultation with healthcare professionals. However, several scenarios and factors might prompt individuals and their healthcare teams to explore alternatives:
Considering an alternative to insulin injections is a decision that should be made in close consultation with healthcare professionals. However, several scenarios and factors might prompt individuals and their healthcare teams to explore alternatives:
- Needle Phobia: Individuals who have a significant fear of needles or experience anxiety related to injections might benefit from exploring alternatives that reduce or eliminate the need for needle use.
- Lifestyle Considerations: For people who lead active lifestyles or travel frequently, the convenience of not having to administer injections multiple times a day may be appealing.
- Difficulty Managing Blood Sugar Levels: Some people may struggle to maintain stable blood sugar levels with injections due to variability in absorption or challenges with dosing. Continuous insulin delivery systems can provide more consistent blood glucose control.
- Injection Site Issues: Repeated injections can lead to issues such as scar tissue, lipodystrophy (changes in fat tissue), or irritation at the injection site. Alternatives can help alleviate or avoid these complications.
- Seeking Improved Blood Sugar Control: Those who have difficulty achieving their target blood glucose levels with injections may find that alternatives offer a better mechanism for tight blood sugar management, especially with the aid of technology like continuous glucose monitoring systems.
- Pediatric Patients: Children with diabetes or their caregivers might prefer alternatives to injections to minimize the emotional and physical burden of daily needle use.
It’s important to note that while alternatives to insulin injections can offer many benefits, they may not be suitable for everyone. The decision to switch should consider factors like the type and severity of diabetes, individual health conditions, and personal preferences.
What Are Some Alternatives to Insulin Injections?
In addition to technological advancements in insulin delivery methods, there are various medications and drugs available for managing diabetes that can serve as alternatives to insulin injections. These alternatives are particularly relevant for people with type 2 diabetes, where a combination can effectively manage the condition. Here’s an overview:
GLP-1 Receptor Agonists
These are injectable medications that mimic the action of the glucagon-like peptide-1 hormone. It helps lower blood sugar levels. They slow gastric emptying, reduce postprandial glucagon release, and stimulate insulin secretion when glucose levels are high. GLP-1 receptor agonists also have the benefit of promoting weight loss. Examples include exenatide (Byetta), liraglutide (Victoza), and semaglutide (Ozempic).
DPP-4 Inhibitors
These oral medications work by blocking the action of the dipeptidyl peptidase-4 enzyme, which leads to an increase in incretin levels (GLP-1 and GIP), enhancing the release of insulin and decreasing the release of glucagon. This results in a reduction in blood glucose levels. DPP-4 inhibitors are known for their weight-neutral effect and are typically used in type 2 diabetes management. Examples include sitagliptin (Januvia) and linagliptin (Tradjenta).
SGLT2 Inhibitors
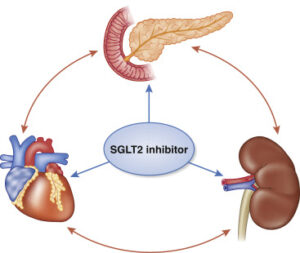 Sodium-glucose cotransporter 2 inhibitors are a class of oral medications that work by preventing the kidneys from reabsorbing glucose back into the blood. This results in the excretion of glucose through the urine, thereby lowering blood sugar levels. Examples include empagliflozin (Jardiance) and dapagliflozin (Farxiga).
Sodium-glucose cotransporter 2 inhibitors are a class of oral medications that work by preventing the kidneys from reabsorbing glucose back into the blood. This results in the excretion of glucose through the urine, thereby lowering blood sugar levels. Examples include empagliflozin (Jardiance) and dapagliflozin (Farxiga).
Sulfonylureas
These are among the oldest oral diabetes medications and work by stimulating the pancreas to release more insulin. This class of drugs can be very effective in lowering blood glucose levels but can also cause hypoglycemia and weight gain, which are significant considerations in their use. Examples include glipizide (Glucotrol) and glyburide (DiaBeta).
Meglitinides
Similar to sulfonylureas, meglitinides stimulate the pancreas to produce more insulin but have a shorter duration of action. They are taken before meals to manage postprandial blood sugar spikes. Because of their short action, the risk of hypoglycemia may be lower compared to sulfonylureas. Examples include repaglinide (Prandin) and nateglinide (Starlix).
Thiazolidinediones (TZDs)
TZDs work by increasing the body’s sensitivity to insulin, allowing the cells to use glucose more effectively. They can be very effective in controlling high blood sugar but have been associated with weight gain, fluid retention, and an increased risk of heart failure. Examples include pioglitazone (Actos) and rosiglitazone (Avandia).
Alpha-glucosidase Inhibitors
These oral medications work by slowing the digestion of carbohydrates in the intestines, which helps to prevent blood sugar spikes after meals. They are less likely to cause hypoglycemia but can cause gastrointestinal side effects. Examples include acarbose (Precose) and miglitol (Glyset).
Bile Acid Sequestrants
Although primarily used to lower cholesterol levels, certain bile acid sequestrants have been approved for use in type 2 diabetes management. They work by binding to bile acids in the intestine. This impacts the regulation of glucose metabolism. One example is colesevelam (Welchol).
Each of these medication classes offers a different mechanism of action for managing diabetes and can be used in various combinations or as an alternative to insulin therapy, depending on the individual’s specific needs and health profile. Individuals with diabetes need to work closely with their healthcare provider to determine the best treatment plan for their situation.
Which Foods Are High In Insulin?
 Foods themselves do not contain insulin, as insulin is a hormone produced by the pancreas in animals, including humans. However, certain foods can influence the body’s insulin response or help manage blood sugar levels. This is particularly important for people with diabetes or insulin resistance. Here are some categories of foods that are beneficial in this regard:
Foods themselves do not contain insulin, as insulin is a hormone produced by the pancreas in animals, including humans. However, certain foods can influence the body’s insulin response or help manage blood sugar levels. This is particularly important for people with diabetes or insulin resistance. Here are some categories of foods that are beneficial in this regard:
- High-Fiber Foods: Foods rich in fiber, such as vegetables, fruits, whole grains, and legumes, can help slow down the digestion of carbohydrates and the absorption of sugar, leading to a more gradual rise in blood sugar and insulin levels.
- Healthy Fats: Consuming foods high in healthy fats, like avocados, nuts, seeds, and olive oil, can help improve insulin sensitivity. These foods do not spike insulin levels because fats do not directly impact blood sugar levels.
- Lean Proteins: Sources of lean protein, such as chicken, fish, tofu, and legumes, can be beneficial for blood sugar control. Protein helps to slow carbohydrate absorption and can increase feelings of fullness, potentially preventing overeating and excessive insulin release.
- Antioxidant-Rich Foods: Foods high in antioxidants, such as berries, leafy greens, and spices like turmeric and cinnamon, may help improve insulin sensitivity and protect against oxidative stress, which is linked to insulin resistance.
- Whole Grains: Whole grains like oats, barley, quinoa, and brown rice have a lower glycemic index than refined grains and can help maintain steady blood sugar levels and improve insulin sensitivity.
- Vinegar: Vinegar, especially apple cider vinegar, can improve insulin sensitivity and lower blood sugar levels after meals. It’s thought to slow the digestion of carbohydrates, contributing to a more gradual insulin response.
- Chromium- and Magnesium-Rich Foods: Minerals like chromium and magnesium are involved in carbohydrate metabolism and insulin action. Foods high in these nutrients, such as broccoli, nuts, whole grains, and dark chocolate, may help improve insulin sensitivity.
- Omega-3 Fatty Acids: Foods rich in omega-3 fatty acids, like fatty fish (salmon, mackerel, sardines), flaxseeds, and chia seeds, are linked to improved insulin sensitivity and reduced inflammation.
While these foods can support blood sugar management and insulin sensitivity, they do not contain insulin themselves. For individuals with diabetes, it’s important to follow a healthcare provider’s advice.
Conclusion
In conclusion, managing diabetes goes beyond just insulin injections. Numerous alternatives to insulin injections include medications and dietary strategies to support insulin sensitivity. Also, helps control blood sugar levels. Foods high in fiber, healthy fats, lean proteins, and antioxidants can improve your body’s response to insulin. However, certain medications can offer different mechanisms of action to manage diabetes effectively.
Hence, work closely with healthcare professionals to find the best treatment plan tailored to your needs. Incorporating these strategies into your lifestyle can improve blood sugar control and enhance your overall health. Do you want to get rid of diabetes? Join our online diabetes treatment program and reverse Diabetes naturally through lifestyle changes such as a Personalized Diet plan, Exercise, Yoga, dieticians, and health coaches.

