Type 2 diabetes is a chronic condition characterized by insulin resistance and impaired insulin secretion. It affects millions worldwide and requires careful management to prevent complications and maintain quality of life. While lifestyle changes, oral medications, and injectable therapies like GLP-1 receptor agonists are commonly used to manage the disease, insulin treatment plays a crucial role in certain situations. In this article, we delve into the intricacies of insulin treatment for type 2 diabetes, its mechanisms, benefits, challenges, and considerations.
Contents
Relationship Between Insulin Resistance and Type 2 Diabetes

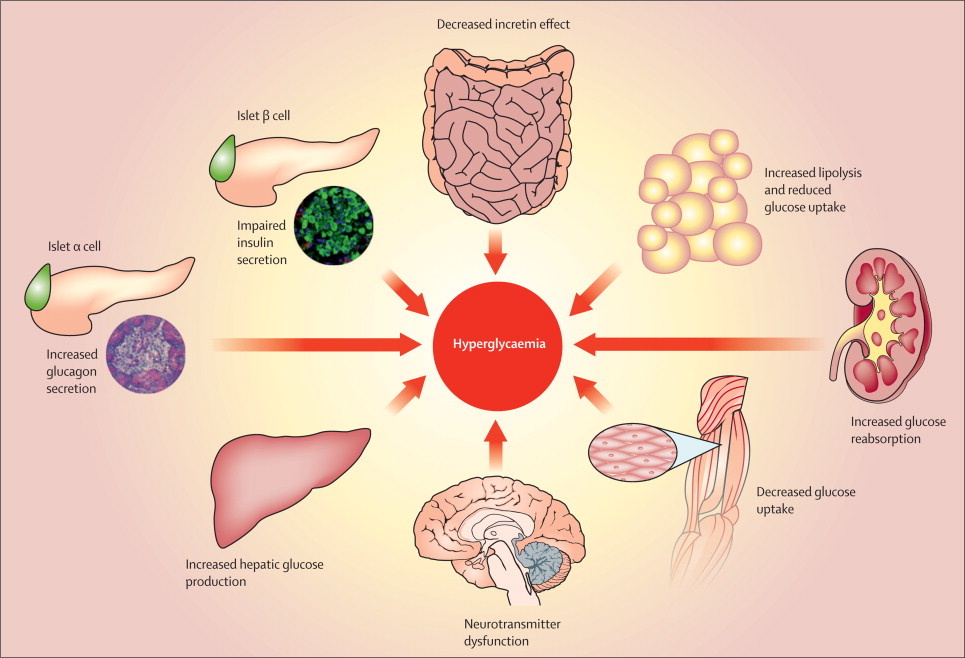
Insulin resistance stands as a cornerstone in the pathophysiology of type 2 diabetes, playing a pivotal role in its development and progression. It refers to the diminished sensitivity of target tissues, such as muscle, liver, and adipose tissue, to the actions of insulin. In essence, insulin resistance disrupts the body’s ability to regulate blood sugar effectively, leading to persistently elevated glucose levels, a hallmark of type 2 diabetes.
At the cellular level, insulin resistance arises due to aberrations in insulin signaling pathways, often exacerbated by various factors including genetic predisposition, obesity, physical inactivity, and aging. Adipose tissue dysfunction, particularly in the setting of excess adiposity, contributes significantly to insulin resistance by releasing increased levels of free fatty acids and pro-inflammatory cytokines. These circulating factors interfere with insulin signaling, impairing glucose uptake and utilization in peripheral tissues.
As insulin resistance progresses, pancreatic beta cells ramp up insulin production in an attempt to overcome the diminished tissue sensitivity. Initially, this compensatory response helps maintain normal blood glucose levels. However, prolonged exposure to elevated glucose and fatty acids can lead to beta-cell dysfunction and impaired insulin secretion. The resulting decline in beta-cell function further exacerbates hyperglycemia, setting the stage for the onset of type 2 diabetes.
Role of Insulin in Type 2 Diabetes Management
Insulin plays a crucial role in the management of type 2 diabetes, particularly when other treatment modalities fail to achieve adequate glycemic control. Despite being traditionally associated with type 1 diabetes, where insulin production is deficient, its therapeutic benefits extend to type 2 diabetes as well. Here’s a detailed look at the role of insulin in the management of type 2 diabetes:
- Supplementation of Insulin: In type 2 diabetes, insulin resistance, and impaired insulin secretion contribute to elevated blood sugar levels. Insulin therapy supplements the body’s insulin supply, helping to overcome insulin resistance and reduce hyperglycemia. By providing exogenous insulin, therapy aims to mimic the physiological insulin response and normalize blood glucose levels.
- Glycemic Control: Insulin therapy is highly effective in lowering blood glucose levels, thereby reducing the risk of acute and chronic complications associated with hyperglycemia. It helps regulate fasting and postprandial glucose levels, contributing to overall glycemic control and improving long-term outcomes in individuals with type 2 diabetes.
- Customized Treatment Regimens: Various types of insulin formulations are available, each with unique onset, peak action, and duration profiles. This allows for the customization of treatment regimens tailored to individual needs and lifestyle preferences. Options range from rapid-acting insulin for mealtime coverage to long-acting insulin for basal insulin requirements, providing flexibility in diabetes management.
- Combination Therapy: Insulin therapy can be used alone or in combination with oral antidiabetic medications, such as metformin, sulfonylureas, or DPP-4 inhibitors. Combining insulin with other agents may enhance glycemic control and reduce the required insulin dosage, thereby minimizing the risk of hypoglycemia and weight gain associated with insulin monotherapy.
- Preservation of Beta-Cell Function: Early initiation of insulin therapy in type 2 diabetes may help preserve pancreatic beta-cell function by reducing glucotoxicity and lipotoxicity, thereby slowing the progression of the disease. Preserving beta-cell function is essential for maintaining endogenous insulin secretion and minimizing the need for escalating insulin doses over time.
- Management of Hyperglycemic Crises: In cases of severe hyperglycemia or diabetic ketoacidosis (DKA), insulin therapy is indispensable for rapidly lowering blood glucose levels and correcting metabolic imbalances. Intravenous insulin infusion is often employed in hospitalized patients to achieve tight glycemic control and prevent life-threatening complications.
- Cardiovascular Benefits: Some studies suggest that certain insulin formulations, such as insulin glargine, may offer cardiovascular protection in patients with type 2 diabetes. Improved glycemic control and reduced inflammation associated with insulin therapy may contribute to these cardiovascular benefits, although further research is needed to elucidate the mechanisms involved.
Types of Insulin for Type 2 Diabetes

For individuals with type 2 diabetes, various types of insulin are available, each with unique characteristics in terms of onset, peak action, and duration. The choice of insulin type depends on factors such as the individual’s glycemic control, lifestyle, meal patterns, and treatment goals. Here’s an overview of the different types of insulin used in the management of type 2 diabetes:
Rapid-Acting Insulin:
- Examples: Insulin lispro (Humalog), Insulin aspart (NovoLog), Insulin glulisine (Apidra).
- Onset: Rapid, typically within 15 minutes of administration.
- Peak Action: Peaks within 1 to 2 hours.
- Duration: Last for about 3 to 4 hours.
- Administration: Injected subcutaneously just before or immediately after meals to control postprandial glucose spikes.
Short-Acting Insulin (Regular Insulin):
- Examples: Regular insulin (Humulin R, Novolin R).
- Onset: Begins working within 30 minutes of administration.
- Peak Action: Peaks in 2 to 3 hours.
- Duration: Last for about 6 to 8 hours.
- Administration: Injected subcutaneously 30 to 60 minutes before meals to cover the rise in blood sugar that occurs after eating.
Intermediate-Acting Insulin:
- Examples: Neutral protamine Hagedorn (NPH) insulin (Humulin N, Novolin N).
- Onset: Onset occurs within 1 to 2 hours.
- Peak Action: Peaks in 4 to 12 hours.
- Duration: Last for about 12 to 18 hours.
- Administration: Typically injected one to two times daily to provide basal insulin coverage, often combined with rapid- or short-acting insulin before meals.
Long-Acting Insulin:
- Examples: Insulin glargine (Lantus, Basaglar), Insulin detemir (Levemir), Insulin degludec (Tresiba).
- Onset: Takes several hours to start working.
- Peak Action: Minimal or no pronounced peak.
- Duration: Last for up to 24 hours or longer.
- Administration: Usually injected once daily to provide basal insulin coverage, helping to maintain stable blood sugar levels throughout the day and night.
Ultra-Long-Acting Insulin:
- Example: Insulin degludec (Tresiba).
- Onset: Slow and steady onset.
- Peak Action: Flat and steady action profile over 24 hours or more.
- Duration: Last for more than 24 hours.
- Administration: Injected once daily at any time of the day, offering flexibility in dosing timing.
In addition to these traditional insulin formulations, premixed insulin products combining rapid-acting or short-acting insulin with intermediate-acting insulin are also available, offering convenience for individuals who require both basal and prandial insulin coverage.
Initiating Insulin Therapy in Type 2 Diabetes: Insulin therapy is typically initiated when blood sugar levels remain uncontrolled despite lifestyle modifications and oral medications. Factors influencing the decision to start insulin include HbA1c levels, fasting, and postprandial glucose levels, presence of symptoms, patient’s willingness, and potential risks and benefits.
Benefits of Insulin Resistance for Type 2 Diabetes

Insulin resistance is a fundamental characteristic of type 2 diabetes, representing a state where target tissues exhibit reduced responsiveness to the actions of insulin. While insulin resistance is typically viewed as a detrimental aspect of type 2 diabetes pathophysiology, there are some potential benefits associated with this phenomenon:
- Survival Advantage in Certain Environments: In ancestral environments characterized by food scarcity and periods of fasting, insulin resistance may have conferred a survival advantage. Individuals with insulin resistance were better equipped to conserve glucose for essential organs such as the brain during times of limited food availability. This evolutionary perspective suggests that insulin resistance may have served as an adaptive trait in specific environmental contexts.
- Energy Storage Mechanism: Insulin resistance is often accompanied by increased lipolysis and elevated circulating levels of free fatty acids. While excessive lipid accumulation in non-adipose tissues can contribute to metabolic dysfunction, it also serves as an energy storage mechanism during times of plenty. In adipose tissue, insulin resistance promotes the storage of excess calories as triglycerides, buffering against fluctuations in nutrient availability.
- Protective Role Against Hypoglycemia: In individuals with insulin resistance, higher fasting insulin levels help maintain adequate blood glucose levels and reduce the risk of hypoglycemia, especially during periods of prolonged fasting or low carbohydrate intake. The compensatory hyperinsulinemia observed in insulin-resistant states helps counteract the diminished tissue sensitivity to insulin and ensures glucose homeostasis.
- Increased Muscle Mass: Insulin resistance is associated with compensatory hyperinsulinemia, which stimulates the mTOR (mechanistic target of rapamycin) pathway and promotes muscle protein synthesis. As a result, individuals with insulin resistance may exhibit greater muscle mass and strength compared to their insulin-sensitive counterparts. This phenomenon may confer metabolic benefits, as skeletal muscle serves as a major site for glucose disposal and insulin action.
- Potential Protective Effect Against Neurodegenerative Diseases: Some studies suggest that insulin resistance may confer neuroprotective effects and reduce the risk of neurodegenerative diseases such as Alzheimer’s disease. Insulin resistance in the brain may enhance neuronal survival and plasticity, thereby mitigating cognitive decline associated with aging and neurodegeneration.
Challenges and Considerations for Insulin Resistance for Type 2 Diabetes
Insulin resistance poses significant challenges and considerations in the management of type 2 diabetes, affecting both patients and healthcare providers. Addressing these challenges is essential for optimizing treatment outcomes and reducing the risk of complications associated with insulin resistance. Here are some key considerations:
- Poor Glycemic Control: Insulin resistance contributes to elevated blood glucose levels by impairing insulin-mediated glucose uptake in peripheral tissues. Despite compensatory hyperinsulinemia, individuals with insulin resistance may struggle to achieve target glycemic control, leading to an increased risk of microvascular and macrovascular complications associated with hyperglycemia.
- Increased Risk of Cardiovascular Disease: Insulin resistance is a major risk factor for cardiovascular disease, independently contributing to endothelial dysfunction, dyslipidemia, hypertension, and inflammation. These metabolic abnormalities collectively elevate the risk of atherosclerosis, myocardial infarction, stroke, and other cardiovascular events in individuals with type 2 diabetes.
- Progressive Nature of Insulin Resistance: Insulin resistance tends to worsen over time, particularly in the setting of obesity, physical inactivity, and aging. Progressive insulin resistance exacerbates beta-cell dysfunction and impairs insulin secretion, leading to further deterioration of glycemic control and necessitating escalation of treatment strategies to maintain target blood glucose levels.
- Risk of Hypoglycemia: Compensatory hyperinsulinemia in insulin-resistant states increases the risk of hypoglycemia, especially when insulin therapy starts. Insulin-resistant individuals may require higher insulin doses to achieve glycemic targets, predisposing them to hypoglycemic episodes if dosages are not adjusted appropriately or if meal timings change.
- Weight Gain and Obesity: Insulin resistance associates with obesity and visceral adiposity, contributing to a vicious cycle of worsening insulin resistance and weight gain. Excess adiposity exacerbates inflammation, promotes insulin resistance, and impairs metabolic health, further complicating the management of type 2 diabetes.
- Multifactorial Etiology: Insulin resistance is a complex and multifactorial condition influenced by genetic, environmental, and lifestyle factors. Addressing insulin resistance requires a comprehensive approach that targets underlying metabolic abnormalities, including obesity, physical inactivity, poor dietary habits, and metabolic syndrome components.
- Psychosocial Impact: Managing insulin resistance and type 2 diabetes can be emotionally challenging for patients, often requiring significant lifestyle modifications, self-monitoring, and adherence to treatment regimens. Psychosocial factors such as diabetes distress, depression, anxiety, and medication adherence issues can further complicate disease management and impact overall well-being.
Conclusion
Insulin therapy plays a vital role in managing type 2 diabetes, especially when other treatments fail to achieve adequate glycemic control. Addressing insulin resistance and supplementing deficient insulin secretion, helps regulate blood sugar levels and reduces the risk of complications. However, initiating insulin therapy requires careful consideration of various factors, and close monitoring is essential to optimize outcomes while minimizing risks. With proper education, support, and adherence to treatment regimens, individuals with type 2 diabetes can effectively incorporate insulin therapy into their diabetes management plan, leading to improved health and well-being.
Do you want to get rid of diabetes? Join our online diabetes treatment program and reverse Diabetes naturally through lifestyle changes such as a Personalized Diet plan, Exercise, Yoga, dieticians, and health coaches.