Diabetes has long been a significant health concern. Characterized by high blood sugar levels due to the body’s inability to produce or properly use insulin, diabetes manifests in various forms, primarily Type 1 and Type 2. While modern medicine has made tremendous strides in managing this condition, the quest for a permanent cure continues to be a topic of immense research and hope. This blog aims to explore the permanent cures for diabetes.
Contents
Will There Be Permanent Cures For Diabetes?
 The possibility of a permanent cure for diabetes remains one of the most fervently pursued goals in medical science. Despite the complexity of the disease, researchers are continuously making significant strides in understanding the underlying mechanisms of both Type 1 and Type 2 diabetes. This deepening understanding is crucial as it lays the foundation for developing more effective treatments.
The possibility of a permanent cure for diabetes remains one of the most fervently pursued goals in medical science. Despite the complexity of the disease, researchers are continuously making significant strides in understanding the underlying mechanisms of both Type 1 and Type 2 diabetes. This deepening understanding is crucial as it lays the foundation for developing more effective treatments.
Current efforts are focused on various aspects of the disease, ranging from prevention strategies to innovative therapies that could offer more sustainable and long-lasting control of blood sugar levels. Moreover, the landscape of diabetes management is rapidly evolving, driven by technological advancements and a better grasp of the disease’s biological underpinnings. While these developments do not yet constitute a cure, they represent significant steps forward in managing the disease more effectively.
What Are The Best Permanent Cures For Diabetes?
Generally, there is no known permanent cure for diabetes. However, significant progress has been made in the development of new therapies and medical approaches that aim to effectively manage, particularly in the case of Type 2 diabetes. Here are some of the permanent cures for diabetes:
Advanced Insulin Therapy
These advanced formulations are designed to mimic the body’s natural insulin release more closely. This approach helps in minimizing the risk of blood sugar spikes and drops, which are common with older insulin types. Long-acting insulins provide a steady level of insulin, reducing the need for frequent injections while fast-acting analogs can more effectively manage blood sugar levels during meals. This development has greatly enhanced the quality of life for people with diabetes.
Bariatric Surgery
For individuals with obesity and Type 2 diabetes, bariatric surgery has emerged as a significant intervention. This surgery alters the gastrointestinal tract, leading to substantial weight loss and often resulting in the remission of Type 2 diabetes. The changes in the digestive system can lead to hormonal changes that improve insulin sensitivity and glucose metabolism. The success of bariatric surgery in managing diabetes highlights the complex relationship between weight, diet, and diabetes.
Islet Cell Transplantation
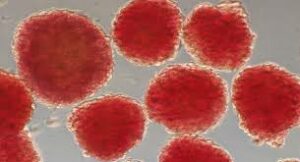 Islet cell transplantation represents a promising frontier for Type 1 diabetes treatment. This procedure involves transplanting islet cells containing insulin-producing beta cells from a donor pancreas into a patient with Type 1 diabetes. Although still considered experimental and facing challenges like limited donor availability and the need for lifelong immunosuppressive drugs to prevent rejection, successful transplantation can lead to the production of natural insulin, reducing or eliminating the need for insulin injections.
Islet cell transplantation represents a promising frontier for Type 1 diabetes treatment. This procedure involves transplanting islet cells containing insulin-producing beta cells from a donor pancreas into a patient with Type 1 diabetes. Although still considered experimental and facing challenges like limited donor availability and the need for lifelong immunosuppressive drugs to prevent rejection, successful transplantation can lead to the production of natural insulin, reducing or eliminating the need for insulin injections.
Stem Cell Therapy
Research in stem cell therapy for Type 1 diabetes focuses on developing insulin-producing cells from stem cells. These cells could then be transplanted into patients, potentially restoring their ability to produce insulin naturally. This approach aims to replace the damaged beta cells that are at the root of Type 1 diabetes. While still in the research and testing phase, stem cell therapy holds great promise as a potential cure, offering a permanent solution to insulin dependence.
Immunotherapy
Immunotherapy for Type 1 diabetes involves modulating the immune system’s response. This leads to the destruction of insulin-producing cells. Various strategies are being researched, including drugs that could halt or slow the autoimmune attack on pancreatic cells. This approach aims to preserve and protect the remaining insulin-producing cells, potentially changing the course of the disease and reducing insulin dependence.
Artificial Pancreas Systems
Artificial pancreas systems are a significant breakthrough in Type 1 diabetes management. These systems integrate continuous glucose monitoring with automated insulin delivery, effectively simulating a healthy pancreas. The device continuously monitors blood glucose levels and automatically adjusts insulin delivery. And, providing a more precise and responsive way to manage blood sugar levels, significantly reducing the burden of constant monitoring and adjustment typically required by patients.
GLP-1 Receptor Agonists and SGLT2 Inhibitors
For Type 2 diabetes, newer classes of medications like GLP-1 receptor agonists and SGLT2 inhibitors have become increasingly popular. These drugs work in different ways to help control blood sugar levels. GLP-1 receptor agonists mimic a natural hormone to stimulate insulin production and decrease appetite, often leading to weight loss. SGLT2 inhibitors help the kidneys lower blood sugar levels by excreting excess glucose through urine.
It’s important to note that while these therapies and approaches can be highly effective in managing diabetes, they are not universally considered permanent cures for diabetes. The effectiveness of each approach can vary greatly from person to person. Hence, ongoing research is needed to develop therapies that could offer a true cure.
What Are Some Natural Cures For Diabetes?
 Diabetes is a chronic condition that requires ongoing management. However, there are natural ways to help manage diabetes and improve overall health, which can be particularly effective in the case of Type 2 diabetes. Here are some methods:
Diabetes is a chronic condition that requires ongoing management. However, there are natural ways to help manage diabetes and improve overall health, which can be particularly effective in the case of Type 2 diabetes. Here are some methods:
Healthy Diet
Focusing on foods low in refined sugars and carbohydrates helps prevent spikes in blood sugar levels. High-fiber foods, such as whole grains, vegetables, fruits, and legumes, slow down the digestion of carbohydrates, leading to a more gradual rise in blood sugar. Incorporating lean proteins and healthy fats found in fish, nuts, seeds, and avocados can also help regulate blood sugar levels. Diets such as the Mediterranean diet, rich in whole foods and low in processed items, are particularly beneficial for individuals with diabetes.
Regular Exercise
Exercise is a powerful tool in diabetes management. Regular physical activity increases insulin sensitivity, meaning your body requires less insulin to transport sugar to your cells. A mix of aerobic exercises like walking, cycling, swimming, and strength training is often recommended. Individuals with diabetes need to find a form of exercise they enjoy and can maintain regularly. Even daily activities like gardening or taking the stairs can contribute to better blood sugar control.
Weight Management
For those with Type 2 diabetes or prediabetes, weight management is crucial. Losing even a small percentage of body weight can significantly improve blood sugar control and reduce the risk of developing diabetes-related complications. This can be achieved through a combination of diet and exercise. And sometimes in consultation with a dietitian or a healthcare provider.
Herbal Remedies and Supplements
Certain herbs and supplements are thought to help improve insulin sensitivity or lower blood sugar. For example, cinnamon has been studied for its potential to lower blood sugar levels. Bitter melon, fenugreek, and alpha-lipoic acid are other supplements that some studies have suggested might help with blood sugar control. However, it’s important to approach these remedies cautiously and always consult with a healthcare professional.
Stress Management
Stress can have a significant impact on blood sugar levels. Techniques like meditation, yoga, and deep breathing exercises can help reduce stress. Regular practice of these activities can lead to better mental health and improved blood sugar control. Cognitive-behavioral therapy (CBT) and other forms of counseling can also be effective in managing diabetes-related stress.
Adequate Sleep
Sleep has a direct effect on blood sugar levels and insulin sensitivity. Poor sleep can disrupt important hormones and cause imbalances that affect how your body manages sugar. Establishing a regular sleep schedule, creating a restful sleeping environment, and avoiding caffeine and electronic devices before bed can help improve sleep quality.
Hydration
Proper hydration is key for overall health and can help in managing diabetes. Drinking sufficient water helps maintain blood sugar levels within a healthy range and supports kidney function. This can be compromised in diabetics. Water is the best choice, and it’s recommended to avoid sugary drinks which can lead to blood sugar spikes.
These methods, while helpful in managing diabetes, are most effective when used in conjunction with traditional medical treatments. Individuals with diabetes need to work closely with their healthcare providers to create a comprehensive treatment plan tailored to their individual needs.
Conclusion
In conclusion, while there are currently no known permanent cures for diabetes, effectively managing the condition is possible through a combination of medical treatment and lifestyle changes. Adopting a healthy diet, staying active with regular exercise, managing weight, and incorporating natural supplements, if advised by a healthcare professional, can make a significant difference.
Remember, these strategies should complement, not replace, medical treatments. Hence, it’s always important to consult with healthcare professionals to tailor a plan that’s right for you. Do you want to get rid of diabetes? Join our online diabetes treatment program and reverse Diabetes naturally through lifestyle changes such as a Personalized Diet plan, Exercise, Yoga, dieticians, and health coaches.

