Diabetes, a chronic condition affecting millions worldwide, has long been a topic of medical research and public health concern. While management strategies such as medication, diet, and exercise play crucial roles in controlling blood sugar levels, the quest for a permanent treatment remains ongoing. In this blog, we delve into the concept of permanent treatment for diabetes, exploring current advancements, challenges, and the potential future landscape of diabetes care.
Contents
What is Diabetes?

Diabetes mellitus, commonly known as diabetes, is a chronic metabolic disorder characterized by elevated levels of glucose (sugar) in the blood. Glucose is a vital source of energy for cells in the body, and its levels are normally regulated by insulin, a hormone produced by the pancreas. However, in diabetes, the body either doesn’t produce enough insulin or doesn’t effectively use the insulin it produces, leading to hyperglycemia (high blood sugar levels).
There are several types of diabetes, including:
- Type 1 Diabetes: Type 1 diabetes, often referred to as juvenile diabetes or insulin-dependent diabetes, typically develops during childhood or adolescence, although it can occur at any age. In Type 1 diabetes, the immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas, leading to a complete deficiency of insulin. Individuals with Type 1 diabetes require lifelong insulin therapy to manage their blood sugar levels.
- Type 2 Diabetes: Type 2 diabetes is the most common form of diabetes, accounting for the majority of cases worldwide. It usually develops in adults, although it is increasingly being diagnosed in children and adolescents due to rising rates of obesity and sedentary lifestyles. In Type 2 diabetes, the body becomes resistant to the effects of insulin, and over time, the pancreas may fail to produce enough insulin to compensate. Lifestyle factors such as obesity, physical inactivity, and poor dietary habits contribute to the development of Type 2 diabetes. Management of Type 2 diabetes often involves lifestyle modifications, oral medications, injectable insulin, and other adjunct therapies.
Is There Any Permanent Treatment Method for Diabetes?
Current Treatment Approaches: Presently, diabetes management primarily revolves around lifestyle modifications, oral medications, injectable insulin, and other adjunct therapies. While these approaches effectively control blood sugar levels and reduce the risk of complications, they do not offer a permanent solution. Individuals with diabetes must adhere to lifelong treatment regimens to maintain optimal health.
There is no widely accepted permanent cure for diabetes. However, several promising research avenues and treatments are being explored, offering hope for improved management and potential long-term solutions. Here are some notable approaches being investigated:
Islet Cell Transplantation
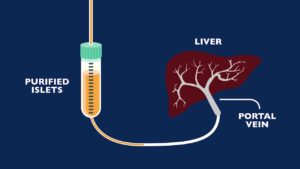
Islet cell transplantation involves implanting insulin-producing cells (islet cells) into the pancreas of individuals with Type 1 diabetes.
While this approach can provide insulin independence for some recipients, it is not widely available and is typically reserved for those with severe hypoglycemia unawareness or other complications of Type 1 diabetes. Challenges include the need for lifelong immunosuppressive therapy to prevent rejection of the transplanted cells and a limited supply of donor islet cells.
Stem Cell Therapy
Stem cell therapy holds promise for regenerating pancreatic beta cells, which are destroyed in Type 1 diabetes. Researchers are exploring various sources of stem cells, including embryonic stem cells, induced pluripotent stem cells (adult cells reprogrammed to behave like embryonic stem cells), and mesenchymal stem cells, to generate new insulin-producing cells.
While still in the experimental stages, stem cell therapy represents a potential avenue for restoring normal pancreatic function in individuals with Type 1 diabetes.
Gene Therapy
Gene therapy aims to correct the genetic defects underlying diabetes, particularly in cases of monogenic diabetes where a single gene mutation contributes to the condition. By introducing functional copies of the defective gene or modifying gene expression, researchers hope to restore normal insulin production and regulation.
While promising, gene therapy for diabetes is still in the early stages of development, with challenges such as ensuring the safety and efficacy of gene delivery methods and addressing ethical considerations.
Artificial Pancreas Technology
The development of closed-loop insulin delivery systems, often referred to as artificial pancreas technology, represents a significant advancement in diabetes care. These systems combine continuous glucose monitoring with automated insulin delivery, mimicking the function of a healthy pancreas by dynamically adjusting insulin doses in response to changing blood sugar levels.
While not a cure, artificial pancreas technology has the potential to revolutionize diabetes management, improving glucose control and quality of life for individuals with Type 1 diabetes.
Benefits of Permanent Treatment Methods for Diabetes

The development of permanent treatment methods for diabetes holds the potential for transformative benefits for individuals living with this chronic condition, as well as for healthcare systems and society as a whole. Here are some of the key benefits that could result from the implementation of permanent treatment methods for diabetes:
Freedom from Daily Management
Perhaps the most significant benefit of a permanent treatment for diabetes is the liberation from the burdensome daily management tasks that individuals with diabetes currently face. These tasks often include frequent blood sugar monitoring, insulin injections or medication administration, carbohydrate counting, and dietary restrictions. A permanent treatment could eliminate or greatly reduce the need for these interventions, allowing individuals to live more freely without the constant worry of managing their condition.
Improved Quality of Life
Managing diabetes can significantly impact an individual’s quality of life, affecting aspects such as physical health, mental well-being, social interactions, and daily activities. A permanent treatment that effectively controls blood sugar levels without the need for ongoing interventions could lead to a substantial improvement in the quality of life for individuals with diabetes. It could alleviate stress, anxiety, and the sense of constant vigilance associated with managing a chronic condition, allowing individuals to focus more on enjoying life and pursuing their goals.
Reduced Risk of Complications
Diabetes is associated with a range of serious complications, including cardiovascular disease, kidney damage, nerve damage, vision loss, and foot problems. Tight control of blood sugar levels is essential for reducing the risk of these complications, but achieving optimal control can be challenging. A permanent treatment that maintains stable blood sugar levels over the long term could help prevent or delay the onset of diabetes-related complications, thereby improving overall health outcomes and reducing healthcare costs.
Less Reliance on Medications
Many individuals with diabetes rely on medications such as insulin injections or oral antidiabetic drugs to manage their condition. While these medications are effective at controlling blood sugar levels, they may be associated with side effects, adherence challenges, and financial burdens. A permanent treatment that addresses the underlying cause of diabetes could reduce or eliminate the need for these medications, minimizing potential side effects and simplifying treatment regimens.
Long-Term Cost Savings
Diabetes imposes a significant economic burden on healthcare systems and society due to the costs associated with medical care, medications, disability, and lost productivity. By preventing or delaying diabetes-related complications and reducing the need for ongoing management, a permanent treatment could lead to substantial cost savings over the long term. These savings could be reinvested in preventive healthcare measures, research, and other priorities aimed at improving population health.
Empowerment and Empathy
Beyond the tangible benefits, a permanent treatment for diabetes could foster a sense of empowerment and empathy among individuals living with the condition and the broader community. It could inspire hope for a future free from the limitations imposed by diabetes and encourage greater understanding and support for those affected by the disease. By elevating awareness and advocacy efforts, a permanent treatment could catalyze positive social change and contribute to a more inclusive and compassionate society.
Challenges and Considerations for Permanent Treatment Methods for Diabetes
The pursuit of a permanent treatment method for diabetes faces numerous challenges and considerations, ranging from scientific and medical hurdles to ethical and logistical issues. Here are some of the key challenges and considerations:
- Safety and Efficacy: Ensuring the safety and efficacy of any potential permanent treatment for diabetes is paramount. Experimental therapies such as stem cell therapy and gene therapy carry inherent risks, including the potential for adverse effects, immune rejection, and unintended consequences. Rigorous preclinical studies and clinical trials are necessary to evaluate the safety and effectiveness of new treatments before they can be considered for widespread use.
- Long-Term Sustainability: A permanent treatment for diabetes must provide lasting benefits without the need for ongoing intervention or maintenance therapy. Achieving sustained glucose control and preserving pancreatic function over the long term present significant challenges, particularly given the progressive nature of Type 1 and Type 2 diabetes and the potential for relapse or recurrence of hyperglycemia.
- Personalized Medicine: Diabetes is a heterogeneous condition with diverse underlying mechanisms and clinical presentations. A one-size-fits-all approach to treatment is unlikely to be effective for all individuals with diabetes. Personalized medicine strategies, tailored to each patient’s unique genetic, metabolic, and lifestyle factors, will be essential for optimizing treatment outcomes and minimizing adverse effects.
- Accessibility and Affordability: Access to cutting-edge diabetes treatments may be limited by factors such as cost, availability of specialized healthcare facilities, and geographic location. Addressing disparities in access to care and ensuring equitable distribution of new therapies will be critical for maximizing their impact and reaching underserved populations.
- Regulatory Approval and Oversight: New treatments for diabetes must undergo rigorous regulatory review to ensure their safety, efficacy, and quality.
Conclusion
In the quest for a permanent treatment for diabetes, researchers continue to explore innovative approaches aimed at addressing the underlying causes of the condition. While challenges abound, advancements in fields such as stem cell therapy, gene editing, and artificial pancreas technology hold promise for revolutionizing diabetes care in the future.
In the meantime, individuals living with diabetes can take proactive steps to manage their condition effectively through lifestyle modifications, regular monitoring, and adherence to treatment regimens. As science and medicine march forward, the prospect of a world without diabetes grows ever closer.

