Hypoglycemic shock, also known as insulin shock or severe hypoglycemia, is a critical condition that can occur in individuals with diabetes. It results from a drastic drop in blood sugar levels and requires immediate medical attention. This guide aims to provide essential information on recognizing the signs of hypoglycemic shock, understanding its causes, and learning the immediate steps for treatment. Additionally, we will explore preventive measures and long-term management strategies to help those at risk maintain stable blood sugar levels and prevent such emergencies.
Contents
What Is The First Aid Of Hypoglycemia Shock?
 First aid for hypoglycemia (low blood sugar) is crucial, especially for individuals with diabetes, and should be administered promptly to prevent the situation from escalating into a hypoglycemic shock. Here’s a step-by-step guide on how to provide first aid in such situations:
First aid for hypoglycemia (low blood sugar) is crucial, especially for individuals with diabetes, and should be administered promptly to prevent the situation from escalating into a hypoglycemic shock. Here’s a step-by-step guide on how to provide first aid in such situations:
1. Recognize the Symptoms
Be aware of the early signs of hypoglycemia. This can include shakiness, sweating, hunger, irritability, dizziness, headache, blurred vision, rapid heartbeat, or sudden mood changes.
2. Check Blood Sugar Levels
If possible, check the person’s blood sugar level to confirm hypoglycemia. A reading below 70 mg/dL is generally considered low and requires immediate attention.
3. Administer Fast-Acting Sugar
If the person is conscious and able to swallow, provide a fast-acting source of sugar. This could be:
- Glucose tablets or gels (as per the recommended dosage)
- 4 ounces (about 1/2 cup) of regular soda (not diet)
- 4 ounces of fruit juice
- A tablespoon of sugar, honey, or corn syrup
4. Recheck Blood Sugar Levels
After about 15 minutes, recheck their blood sugar. If it remains low (under 70 mg/dL) or if symptoms persist, administer another dose of fast-acting sugar.
5. Provide a Snack or Meal
Once the blood sugar level stabilizes, if it’s going to be an hour or more until their next meal, they should eat a longer-acting carbohydrate and protein source, like a sandwich or a banana with peanut butter.
6. Monitor the Person
Continuously monitor the person. If they do not improve rapidly, or if they lose consciousness, have seizures, or exhibit other severe symptoms, it’s crucial to seek emergency medical help immediately.
Remember, these steps are for guidance and should not replace medical advice. Training in first aid and emergency response is recommended for those who regularly interact with individuals at risk of hypoglycemia.
What Are The Medical Hypoglycemic Shock Treatment?
Medical hypoglycemic shock treatment, particularly in severe cases where the individual is unconscious or unable to take glucose orally, involves several critical steps:
Emergency Medical Services
In severe cases of hypoglycemic shock, immediate medical intervention is critical. This typically involves calling emergency services, such as 911 in the United States, to ensure prompt medical assistance. Emergency responders are trained to handle such crises and can provide rapid, life-saving interventions during transport to a medical facility. This quick response is vital, as prolonged hypoglycemia can lead to irreversible brain damage or even death.
Glucagon Injection
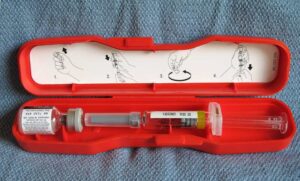 Glucagon is a hormone that counteracts the effects of insulin by raising blood sugar levels. In cases where the individual is unconscious or unable to ingest oral glucose, a bystander or caregiver who is trained can administer a glucagon injection. Glucagon kits are typically prescribed to people at high risk of severe hypoglycemia and should be readily available. The injection can be given intramuscularly or subcutaneously and works by stimulating the liver to release stored glucose into the bloodstream.
Glucagon is a hormone that counteracts the effects of insulin by raising blood sugar levels. In cases where the individual is unconscious or unable to ingest oral glucose, a bystander or caregiver who is trained can administer a glucagon injection. Glucagon kits are typically prescribed to people at high risk of severe hypoglycemia and should be readily available. The injection can be given intramuscularly or subcutaneously and works by stimulating the liver to release stored glucose into the bloodstream.
Intravenous (IV) Glucose
In a hospital or emergency setting, healthcare professionals may administer glucose directly into the bloodstream through an intravenous line. IV glucose acts quickly to raise blood sugar levels. This method is preferred for individuals who are unconscious or in severe hypoglycemic shock, as it bypasses the digestive system and allows for an immediate increase in blood sugar levels.
Monitoring
Continuous monitoring of the individual’s blood sugar levels is crucial following the initial treatment. This monitoring helps to ensure that the blood sugar level is returning to and remaining within a normal range. It also aids in determining if additional glucose administration is necessary. Continuous glucose monitoring can also provide insights into the patient’s response to treatment and recovery progress.
Assessment and Stabilization
In addition to treating hypoglycemia, medical professionals will assess and stabilize other vital signs, such as heart rate, blood pressure, and oxygen saturation. They will also address any complications that may have arisen due to the severe hypoglycemia, such as neurological impairment or cardiac disturbances. This comprehensive assessment is critical to ensure the patient’s overall stability and recovery.
Determination of Cause
Identifying the underlying cause of the hypoglycemic event is essential, particularly for patients with diabetes. This may involve a review of the individual’s medication regimen, including insulin or other hypoglycemic agents, dietary habits, exercise patterns, and recent illnesses or changes in routine. Understanding the cause is crucial for preventing future episodes.
Adjustment of Diabetes Management Plan
For diabetic patients, it may be necessary to adjust their diabetes management plan to prevent future hypoglycemic events. This could include modifications to their insulin therapy, changes in oral diabetic medications, dietary adjustments, and lifestyle changes. Education on more effective blood glucose monitoring and recognizing early signs of hypoglycemia is also typically provided.
Education and Follow-Up
Patient education is a critical component of treatment. This includes educating the patient and their family or caregivers about recognizing early signs of hypoglycemia, how to respond to these signs, and how to administer glucagon if necessary. Regular follow-up visits with a healthcare provider or a diabetes educator are recommended to ensure that the patient is effectively managing their condition and to make further adjustments to their treatment plan as needed.
Each of these steps plays a crucial role in the effective treatment and management of hypoglycemic shock, ensuring not only the immediate safety of the patient but also their long-term health and quality of life.
How Can I Prevent Hypoglycemic Shock?
 Preventing hypoglycemic shock involves a combination of careful management of diabetes (if applicable), lifestyle modifications, and proactive monitoring. Here are several strategies that can help in preventing hypoglycemic shock:
Preventing hypoglycemic shock involves a combination of careful management of diabetes (if applicable), lifestyle modifications, and proactive monitoring. Here are several strategies that can help in preventing hypoglycemic shock:
Consistent Carbohydrate Intake
Eating carbohydrates consistently throughout the day can prevent sudden spikes or drops in blood sugar levels. It’s important to avoid skipping meals and to try to eat at regular intervals. This consistency helps the body to better regulate blood sugar levels, particularly for individuals taking insulin or other diabetes medications.
Balanced Diet
A diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats can contribute to overall good health and stable blood sugar levels. This balanced approach to eating ensures that the body gets the necessary nutrients and energy. This is essential for preventing hypoglycemia.
Regular Blood Sugar Monitoring
Frequent monitoring of blood sugar levels is key, especially for those on insulin or medications that increase insulin production. This regular checking can help in identifying low blood sugar levels early and taking steps to correct them before they lead to hypoglycemia.
Adjust Medication as Necessary
Medications, particularly those for diabetes, may need adjustments based on daily routines, dietary changes, or overall health status. It’s vital to consult with healthcare providers before making any changes, as improper adjustments can lead to hypoglycemia.
Education on Hypoglycemia Management
Being well-informed about the symptoms of hypoglycemia and its management is critical. Understanding how to respond appropriately to low blood sugar levels, including the administration of fast-acting carbohydrates, is a key aspect of prevention.
Exercise Smartly
Exercise is important for overall health and blood sugar control. However, it’s vital to balance physical activity with proper nutrition and, if necessary, medication adjustments. Monitoring blood sugar levels before, during, and after physical activity can help prevent exercise-induced hypoglycemia.
Alcohol Consumption with Caution
Alcohol can significantly impact blood sugar levels and should be consumed cautiously, especially for individuals at risk of hypoglycemia. It’s advisable to consume alcohol with food to mitigate its blood sugar-lowering effects.
Be Prepared
Carrying fast-acting glucose sources such as glucose tablets, candy, or juice is essential, particularly when away from home. This ensures that a quick remedy is at hand in case of sudden hypoglycemia.
Wear a Medical Alert Bracelet
Wearing a medical alert bracelet or carrying an identification card that indicates diabetes can be life-saving in emergencies. This informs responders of your condition, enabling them to provide appropriate care quickly.
Regular Healthcare Checkups
Regular visits to a healthcare provider are essential for monitoring diabetes management and overall health. These checkups provide opportunities to adjust treatment plans, discuss challenges, and receive guidance on preventing hypoglycemia.
Implementing these strategies can significantly help in reducing the risk of hypoglycemic shock. It’s important to remember that these are preventive measures and should be tailored to individual needs and circumstances, often in consultation with healthcare professionals.
Conclusion
In conclusion, hypoglycemic shock treatment involves a multi-faceted approach that includes understanding the condition and knowing the immediate steps to take in case of an emergency. Whether you’re living with diabetes or caring for someone who is, it’s crucial to maintain a balanced diet, monitor blood sugar levels regularly, adjust medications as necessary, and be prepared with fast-acting sources of glucose.
By taking these proactive steps, you can significantly reduce the risk of hypoglycemic shock and lead a healthy, active life. Do you want to get rid of diabetes? Join our online diabetes treatment program and reverse Diabetes naturally through lifestyle changes such as a Personalized Diet plan, Exercise, Yoga, dieticians, and health coaches.

