Diabetes mellitus, a chronic metabolic disorder characterized by elevated blood sugar levels, affects millions worldwide. Managing diabetes involves a multifaceted approach, with lifestyle modifications and medication being key components. Among these medications, first-line treatments are pivotal in controlling blood sugar levels effectively. In this blog, we delve into the various first-line treatment for diabetes, their mechanisms of action, benefits, and considerations for patients and healthcare providers.
Contents
Is there a Need for First-Line Treatment for Diabetes?
There is a critical need for first-line treatment for diabetes. Diabetes is a chronic condition that affects millions of people worldwide and can lead to serious complications if not properly managed. Here are several reasons why first-line treatment for Diabetes is essential:
Control of Blood Sugar Levels
Elevated blood sugar levels are the hallmark of diabetes and can lead to various complications such as heart disease, stroke, kidney disease, nerve damage, and vision problems. First-line treatments, such as metformin and lifestyle modifications, aim to lower blood sugar levels and prevent these complications from occurring.
Early Intervention
Initiating treatment early after diagnosis can help slow down the progression of diabetes and improve long-term outcomes. First-line treatments are often recommended at the time of diagnosis to establish good glycemic control and minimize the risk of complications.
Prevention of Complications
Diabetes complications can be debilitating and significantly impact the quality of life. By effectively managing blood sugar levels with first-line treatments, individuals with diabetes can reduce their risk of developing complications such as cardiovascular disease, neuropathy, nephropathy, and retinopathy.
Improvement of Overall Health
First-line treatments not only target blood sugar control but also promote overall health and well-being. Lifestyle modifications such as healthy eating, regular exercise, and weight management have numerous benefits beyond glycemic control, including improved cardiovascular health, increased energy levels, and enhanced mood.
Cost-Effectiveness
Many first-line treatments, such as metformin and lifestyle modifications, are cost-effective compared to other diabetes medications or medical interventions. By prioritizing these interventions, healthcare systems can reduce the economic burden of diabetes and allocate resources more efficiently.
Patient Empowerment
Empowering individuals with diabetes to take control of their health through first-line treatments fosters a sense of self-efficacy and responsibility. By actively participating in their care and making positive lifestyle changes, patients can improve their health outcomes and quality of life.
List of First-Line Treatment for Diabetes
First-line treatments for diabetes, particularly for type 2 diabetes mellitus (T2DM), are aimed at improving insulin sensitivity, reducing glucose production, and managing blood sugar levels. Here are some of the key first-line treatments commonly used:
Metformin

Metformin stands as the cornerstone of first-line therapy for type 2 diabetes mellitus (T2DM). It belongs to the class of medications known as biguanides and works by reducing glucose production in the liver while enhancing insulin sensitivity in peripheral tissues, such as muscle and fat cells. Metformin does not stimulate insulin secretion from the pancreas, thereby reducing the risk of hypoglycemia. Additionally, it may aid in weight loss or weight maintenance, making it an attractive option for many patients.
Benefits of Metformin:
- Effective in lowering blood sugar levels.
- Low risk of hypoglycemia.
- May promote weight loss.
- Cost-effective compared to other diabetes medications.
- Demonstrated cardiovascular benefits in some studies.
Considerations:
- Gastrointestinal side effects such as nausea, diarrhea, and abdominal discomfort may occur, but they often resolve over time.
- Not recommended in patients with impaired kidney function (creatinine clearance <30 mL/min) due to the risk of lactic acidosis.
- Monitoring of vitamin B12 levels is advised for long-term use.
Lifestyle Modifications
While not strictly medications, lifestyle modifications are integral to the management of diabetes, particularly in the early stages of prediabetes. These modifications include:
- Dietary changes: Emphasizing a balanced diet rich in whole grains, fruits, vegetables, lean proteins, and healthy fats while limiting processed foods, sugars, and refined carbohydrates.
- Regular exercise: Engaging in aerobic exercise, strength training, or other physical activities can improve insulin sensitivity and help control blood sugar levels.
- Weight management: Achieving and maintaining a healthy weight through a combination of diet and exercise can significantly impact diabetes management.
Benefits of Lifestyle Modifications:
- Improves glycemic control.
- Enhances overall health and well-being.
- May reduce the need for medication or insulin therapy.
Considerations:
- Requires commitment and consistency.
- Individualized approach based on patient preferences, cultural factors, and socioeconomic status.
Sodium-Glucose Co-Transporter 2 (SGLT2) Inhibitors
Sodium-glucose co-transporter 2 (SGLT2) inhibitors are a class of medications used primarily in the management of type 2 diabetes mellitus (T2DM).
They work by inhibiting SGLT2, a protein responsible for reabsorbing glucose in the kidneys. By blocking this protein, SGLT2 inhibitors increase urinary glucose excretion, leading to a reduction in blood sugar levels.
- One of the key benefits of SGLT2 inhibitors is their ability to lower blood glucose independently of insulin action, making them particularly useful in patients with T2DM who have insulin resistance or decreased insulin production.
- Additionally, SGLT2 inhibitors have been associated with weight loss due to the loss of calories through increased urinary glucose excretion.
- Beyond their glucose-lowering effects, SGLT2 inhibitors have demonstrated cardiovascular and renal benefits in clinical trials.
- They have been shown to reduce the risk of cardiovascular events, such as heart attacks and strokes, as well as slow the progression of kidney disease in patients with T2DM and established cardiovascular disease or multiple risk factors.
- Commonly prescribed SGLT2 inhibitors include empagliflozin, dapagliflozin, and canagliflozin.
While generally well-tolerated, side effects may consist of genital yeast infections, urinary tract infections, and an increased risk of ketoacidosis, particularly in patients with reduced kidney function. Close monitoring and patient education are essential when prescribing SGLT2 inhibitors to ensure safe and effective management of diabetes.
Dipeptidyl Peptidase-4 (DPP-4) Inhibitors
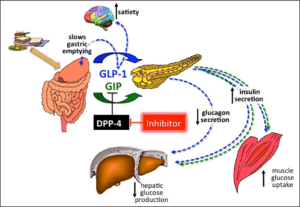
Dipeptidyl peptidase-4 (DPP-4) inhibitors are a class of oral medications used primarily in the treatment of type 2 diabetes mellitus (T2DM).
- They work by inhibiting the enzyme DPP-4, which rapidly degrades incretin hormones such as glucagon-like peptide-1 (GLP-1) and glucose-dependent insulinotropic peptide (GIP).
- By inhibiting DPP-4, these medications prolong the action of incretin hormones, resulting in increased insulin secretion and decreased glucagon release, thereby lowering blood sugar levels.
One of the key benefits of DPP-4 inhibitors is their glucose-lowering effect without significant risk of hypoglycemia, particularly when used as monotherapy or in combination with other oral antidiabetic agents.
They are generally well-tolerated and have a low incidence of adverse effects compared to some other diabetes medications.
- Commonly prescribed DPP-4 inhibitors include sitagliptin, saxagliptin, linagliptin, and vildagliptin.
- These medications are usually taken once daily, with or without food, and are available in various formulations, including tablets and fixed-dose combinations with other antidiabetic agents.
- While DPP-4 inhibitors are effective in improving glycemic control, they may be less potent than some other classes of antidiabetic medications, such as sulfonylureas or insulin.
- Additionally, they may increase the risk of upper respiratory tract infections and nasopharyngitis in some patients.
Glucagon-Like Peptide-1 (GLP-1) Receptor Agonists
Glucagon-like peptide-1 (GLP-1) receptor agonists are a class of medications used primarily in the management of type 2 diabetes mellitus (T2DM). They mimic the action of endogenous GLP-1, a hormone produced in the intestines in response to food intake. GLP-1 plays a crucial role in regulating blood sugar levels by stimulating insulin secretion from pancreatic beta cells, inhibiting glucagon release from pancreatic alpha cells, slowing gastric emptying, and inducing satiety.
By activating the GLP-1 receptor, GLP-1 receptor agonists exert several beneficial effects on glucose metabolism:
- Increased Insulin Secretion: GLP-1 receptor agonists enhance glucose-dependent insulin secretion, meaning they stimulate insulin release only when blood sugar levels are elevated, reducing the risk of hypoglycemia.
- Inhibition of Glucagon Release: They suppress the release of glucagon, a hormone that raises blood sugar levels, particularly in response to fasting or low blood glucose levels.
- Slowed Gastric Emptying: GLP-1 receptor agonists delay the emptying of food from the stomach into the intestines, which helps regulate postprandial blood sugar levels.
- Induction of Satiety: These medications promote feelings of fullness or satiety, which can lead to reduced food intake and potential weight loss.
Commonly prescribed GLP-1 receptor agonists include exenatide, liraglutide, dulaglutide, semaglutide, and lixisenatide. These medications are available in various formulations, including injectable pens or prefilled syringes, as well as oral formulations.
While generally well-tolerated, GLP-1 receptor agonists may cause gastrointestinal side effects such as nausea, vomiting, diarrhea, and constipation, particularly when initiating therapy. They are contraindicated in patients with a history of medullary thyroid carcinoma or multiple endocrine neoplasia syndrome type 2.
Benefits of GLP-1 Receptor Agonists
Key benefits of GLP-1 receptor agonists include:
- Effective Glycemic Control: GLP-1 receptor agonists significantly reduce blood sugar levels, both fasting and postprandial, leading to improved glycemic control in patients with T2DM.
- Weight Loss: Many GLP-1 receptor agonists are associated with weight loss, making them particularly beneficial for overweight or obese individuals with T2DM.
- Cardiovascular Benefits: Some GLP-1 receptor agonists have demonstrated cardiovascular benefits, including reduced risk of cardiovascular events such as heart attacks and strokes, in patients with T2DM and established cardiovascular disease.
- Renal Benefits: Certain GLP-1 receptor agonists have shown renal benefits, including reduced risk of kidney function decline and progression of diabetic kidney disease.
Conclusion
First-line treatments for diabetes encompass a variety of options, ranging from lifestyle modifications to pharmacological interventions such as metformin, SGLT2 inhibitors, DPP-4 inhibitors, and GLP-1 receptor agonists.
Remember, this blog serves as informational content and should not replace professional medical advice. Always consult with a healthcare provider for personalized recommendations and guidance tailored to your specific needs and circumstances.
Do you want to get rid of diabetes? Join our online diabetes treatment program and reverse Diabetes naturally through lifestyle changes such as a Personalized Diet plan, Exercise, Yoga, dieticians, and health coaches.

